Final ID: Sa3050
Distinct Osmolality Trajectories Are Independent Predictors of Adverse in-hospital clinical events in Acute Myocardial Infarction
Abstract Body (Do not enter title and authors here): Background:
Dynamic changes in serum osmolality may reflect fluid imbalance, renal dysfunction, and neurohormonal activation, all of which are relevant in acute myocardial infarction (AMI). However, the prognostic significance of osmolality trajectories in AMI remains unclear.
Objective:
This study aims to investigate the predictive utility of dynamic osmolality trajectories with in-hospital clinical events in AMI.
Methodology:
A retrospective analysis is performed on the MIMIC-IV database. We included 2257 patients with AMI. The median age was 72.0 years (IQR 64.0–81.0), and 1,381 (61.18%) were male. Osmolality is calculated for each day from day 1 to at least day 7 of hospitalization. A Group-based trajectory modeling (GBTM) analysis was performed to identify distinct osmolality trajectories. Our primary outcome is in-hospital mortality, and secondary outcomes are the incidence of congestive heart failure and the incidence of AKI during hospital stay. The association between these trajectories and primary and secondary outcomes was assessed by Firth logistic regression analysis and further adjusted for potential confounders.
Results:
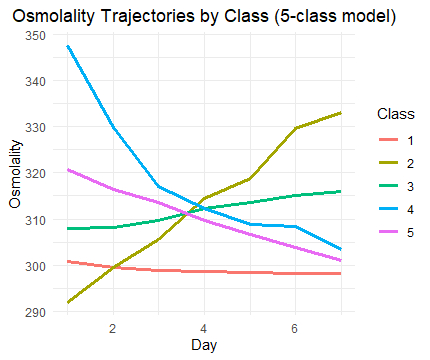
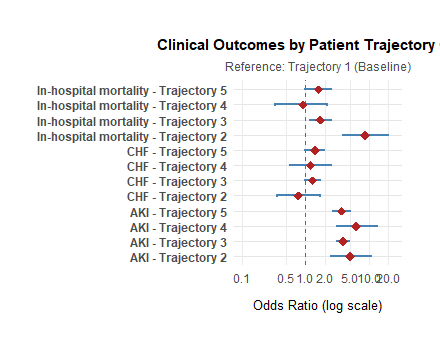
In GBTM analysis, we identified five different trajectories (trajectory 1: low stable-normal, trajectory 2: rapid-increasing, trajectory 3: moderate-increasing, trajectory 4: rapid-decline, trajectory 5: slow-decline). Trajectory 1 is taken as a reference for analysis. After adjusting for covariates, age, gender, temperature, respiratory rate, history of hypertension, hyperlipidemia, cardiogenic shock, AKI, COPD, status of PCI, CABG, beta-blocker, ACEI, and calcium channel blocker, trajectory 2 was strongly associated with higher in-hospital mortality (OR = 8.76, 95% CI: 3.95–19.75; p < 0.001), followed by trajectory 3 (OR = 1.73, 95% CI: 1.20–2.50; p = 0.004). No significant associations were observed for Class 4 (OR = 0.89, 95% CI: 0.33–2.16; p = 0.81) or Class 5 (OR = 1.56, 95% CI: 0.97–2.49; p = 0.07).
No significant association was found between osmolality trajectories and the incidence of CHF. Trends toward increased risk appeared in trajectory 5 (OR = 1.41, p = 0.051) and 3 (OR = 1.29, p = 0.055). All osmolarity trajectories were associated with higher AKI risk. Trajectory 4 (OR = 6.26), trajectory 2 (OR = 5.02), trajectory 3 (OR = 3.92), and trajectory 5 (OR = 3.70) (all p < 0.001).
conclusion:
Dynamic changes in plasma osmolality are a strong predictor of in-hospital clinical events in AMI patients.
Dynamic changes in serum osmolality may reflect fluid imbalance, renal dysfunction, and neurohormonal activation, all of which are relevant in acute myocardial infarction (AMI). However, the prognostic significance of osmolality trajectories in AMI remains unclear.
Objective:
This study aims to investigate the predictive utility of dynamic osmolality trajectories with in-hospital clinical events in AMI.
Methodology:
A retrospective analysis is performed on the MIMIC-IV database. We included 2257 patients with AMI. The median age was 72.0 years (IQR 64.0–81.0), and 1,381 (61.18%) were male. Osmolality is calculated for each day from day 1 to at least day 7 of hospitalization. A Group-based trajectory modeling (GBTM) analysis was performed to identify distinct osmolality trajectories. Our primary outcome is in-hospital mortality, and secondary outcomes are the incidence of congestive heart failure and the incidence of AKI during hospital stay. The association between these trajectories and primary and secondary outcomes was assessed by Firth logistic regression analysis and further adjusted for potential confounders.
Results:
In GBTM analysis, we identified five different trajectories (trajectory 1: low stable-normal, trajectory 2: rapid-increasing, trajectory 3: moderate-increasing, trajectory 4: rapid-decline, trajectory 5: slow-decline). Trajectory 1 is taken as a reference for analysis. After adjusting for covariates, age, gender, temperature, respiratory rate, history of hypertension, hyperlipidemia, cardiogenic shock, AKI, COPD, status of PCI, CABG, beta-blocker, ACEI, and calcium channel blocker, trajectory 2 was strongly associated with higher in-hospital mortality (OR = 8.76, 95% CI: 3.95–19.75; p < 0.001), followed by trajectory 3 (OR = 1.73, 95% CI: 1.20–2.50; p = 0.004). No significant associations were observed for Class 4 (OR = 0.89, 95% CI: 0.33–2.16; p = 0.81) or Class 5 (OR = 1.56, 95% CI: 0.97–2.49; p = 0.07).
No significant association was found between osmolality trajectories and the incidence of CHF. Trends toward increased risk appeared in trajectory 5 (OR = 1.41, p = 0.051) and 3 (OR = 1.29, p = 0.055). All osmolarity trajectories were associated with higher AKI risk. Trajectory 4 (OR = 6.26), trajectory 2 (OR = 5.02), trajectory 3 (OR = 3.92), and trajectory 5 (OR = 3.70) (all p < 0.001).
conclusion:
Dynamic changes in plasma osmolality are a strong predictor of in-hospital clinical events in AMI patients.
More abstracts on this topic:
Artificial Intelligence ECG-Extracted Features Predict Microvascular Obstruction in ST-segment Elevation Myocardial Infarction
Traverse Jay, Meyers Pendell, Sharkey Scott, Schwager Sarah, Stanberry Larissa, Herman Robert
Beyond Closure: A Case Report on Coronary Steal Syndrome by Previously Embolized Internal Mammary Artery Side BranchFuentes Jose, Garcia Almonte Karla, Suero Claudia, Urena Neme Ana Paula, Tarafa Jorge A., Urena V Pedro