Final ID: MP266
Thrombolysis for Minor Non-Disabling Ischemic Stroke: A Meta-analysis of Randomized Controlled Trials
Abstract Body (Do not enter title and authors here): Background: The optimal management of minor ischemic stroke without clearly disabling neurologic deficits remains controversial. Despite the widespread use of intravenous thrombolytic agents in acute ischemic stroke, their role in patients presenting with minor, non-disabling symptoms (National Institutes of Health Stroke Scale [NIHSS] score ≤5) is unclear.
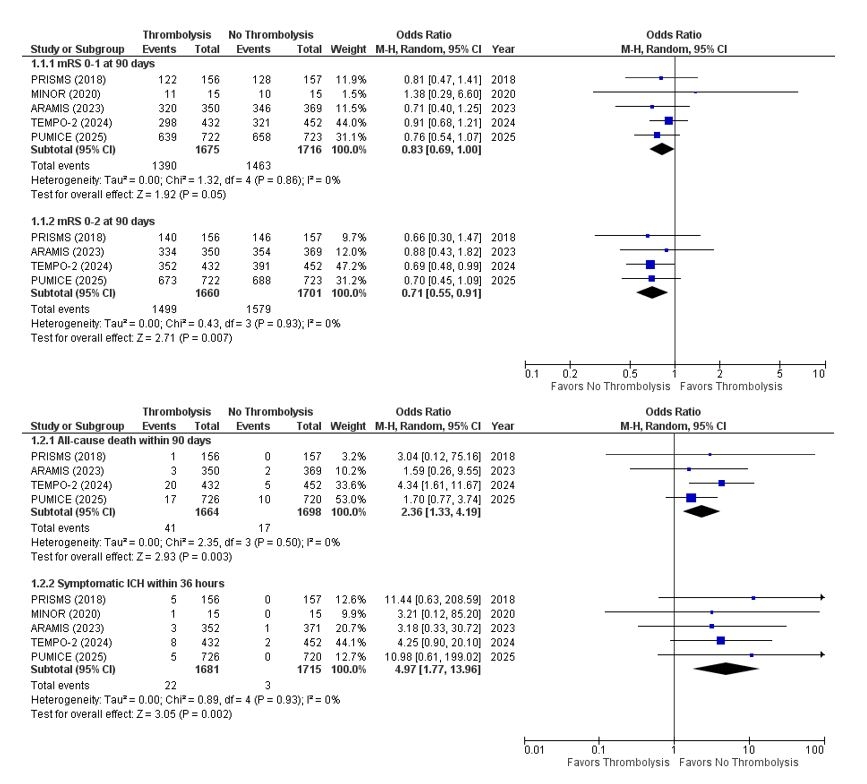
Methods: We conducted a systematic review and meta-analysis of randomized controlled trials (RCTs) comparing intravenous thrombolysis with standard antithrombotic therapy without thrombolysis in patients with minor non-disabling ischemic stroke (NIHSS ≤5) through May 2025. The review protocol was registered in PROSPERO (CRD420251064220). The primary efficacy outcome was excellent functional recovery, defined as modified Rankin Scale (mRS) score 0–1 at 90 days. Secondary efficacy outcomes included functional independence (mRS 0–2) and all-cause death at 90 days. The primary safety outcome was symptomatic intracranial hemorrhage (sICH) within 36 hours of intervention. Odds ratios (OR) and 95% confidence intervals (CI) were calculated using a random-effects model.
Results: A total of five RCTs involving 3,391 patients were included (mean age, 65.8±11.2 years, 36.5% female). Three trials used alteplase (PRISMS, ARAMIS, MINOR), one tenecteplase (TEMPO-2), and one prourokinase (PUMICE). Pooled analysis showed that compared with no thrombolysis, thrombolysis was associated with a lower likelihood of excellent functional outcome (mRS 0–1) (83.0% vs. 85.3%; OR 0.83, 95% CI 0.69–1.00) and functional independence (mRS 0–2) (90.3% vs. 92.8%; OR 0.71, 95% CI 0.55–0.91). Thrombolysis, compared with no thrombolysis, was also associated with higher rates of all-cause mortality (2.5% vs. 1.0%; OR 2.36, 95% CI 1.33–4.19) and sICH (1.3% vs. 0.2%; OR 4.97, 95% CI 1.77–13.96) (Figure).
Conclusion: In patients with minor non-disabling ischemic stroke, thrombolysis was associated with significantly worse clinical outcomes, including reduced functional recovery, higher risk of sICH, and increased mortality. These findings argue against the routine use of thrombolysis in this patient population.
Methods: We conducted a systematic review and meta-analysis of randomized controlled trials (RCTs) comparing intravenous thrombolysis with standard antithrombotic therapy without thrombolysis in patients with minor non-disabling ischemic stroke (NIHSS ≤5) through May 2025. The review protocol was registered in PROSPERO (CRD420251064220). The primary efficacy outcome was excellent functional recovery, defined as modified Rankin Scale (mRS) score 0–1 at 90 days. Secondary efficacy outcomes included functional independence (mRS 0–2) and all-cause death at 90 days. The primary safety outcome was symptomatic intracranial hemorrhage (sICH) within 36 hours of intervention. Odds ratios (OR) and 95% confidence intervals (CI) were calculated using a random-effects model.
Results: A total of five RCTs involving 3,391 patients were included (mean age, 65.8±11.2 years, 36.5% female). Three trials used alteplase (PRISMS, ARAMIS, MINOR), one tenecteplase (TEMPO-2), and one prourokinase (PUMICE). Pooled analysis showed that compared with no thrombolysis, thrombolysis was associated with a lower likelihood of excellent functional outcome (mRS 0–1) (83.0% vs. 85.3%; OR 0.83, 95% CI 0.69–1.00) and functional independence (mRS 0–2) (90.3% vs. 92.8%; OR 0.71, 95% CI 0.55–0.91). Thrombolysis, compared with no thrombolysis, was also associated with higher rates of all-cause mortality (2.5% vs. 1.0%; OR 2.36, 95% CI 1.33–4.19) and sICH (1.3% vs. 0.2%; OR 4.97, 95% CI 1.77–13.96) (Figure).
Conclusion: In patients with minor non-disabling ischemic stroke, thrombolysis was associated with significantly worse clinical outcomes, including reduced functional recovery, higher risk of sICH, and increased mortality. These findings argue against the routine use of thrombolysis in this patient population.
More abstracts on this topic:
1-Year Outcomes After Cardioversion With and Without Anticoagulation in Patients With Left Atrial Appendage Occlusion: A Propensity-Matched Analysis
Thangjui Sittinun, Trongtorsak Angkawipa, Kewcharoen Jakrin, Thyagaturu Harshith, Watson Hangyu, Mensah Samuel, Balla Sudarshan, Navaravong Leenhapong
A Contactless and Automated Approach to the Acute Stroke AssessmentSaadat Moh, Titus Ryan, Verkuilen Haley, Fleming Phil, Sur Sanjib, Sen Souvik