Final ID: MP1018
Device Therapy in Cardiac Sarcoidosis: A Comparative Analysis of ICD and PPM on Mortality, Hospitalization, and Incident Heart Failure
Abstract Body (Do not enter title and authors here): Background:
Patients with cardiac sarcoidosis (CS) generally have a poor prognosis, due to an increased risk for arrhythmias, heart failure (HF), and sudden cardiac death often necessitating device therapy. However, in patients with preserved left ventricular ejection fraction (LVEF), the optimal device—implantable cardioverter-defibrillator (ICD) vs. permanent pacemaker (PPM)—remains unclear. Our study assessed the impact of ICD vs. PPM in CS on clinical outcomes, including mortality, hospitalization, and HF development in this population.
Objective:
Evaluate mortality, hospitalization, and development of HF in patients with CS and normal LVEF who received an ICD vs PPM.
Methods:
We conducted a retrospective cohort analysis using the TriNetX Research Network, which aggregates electronic health records from 102 healthcare organizations. Adult patients (≥18 years) with CS and a LVEF > 35% receiving either an ICD (n=1,403) or PPM (n=115) after initial diagnosis were included. Patients with reduced LVEF and prior ventricular tachycardia were excluded. Propensity score matching (1:1) was used to adjust for baseline differences across 12 demographic, clinical, and laboratory variables (n = 113 in each group). The primary outcomes were all-cause mortality, hospitalizations, and incidence of HF following device implantation. Risk ratios, Kaplan-Meier survival analysis, hazard ratios, and p-values were used for comparative analysis.
Results:
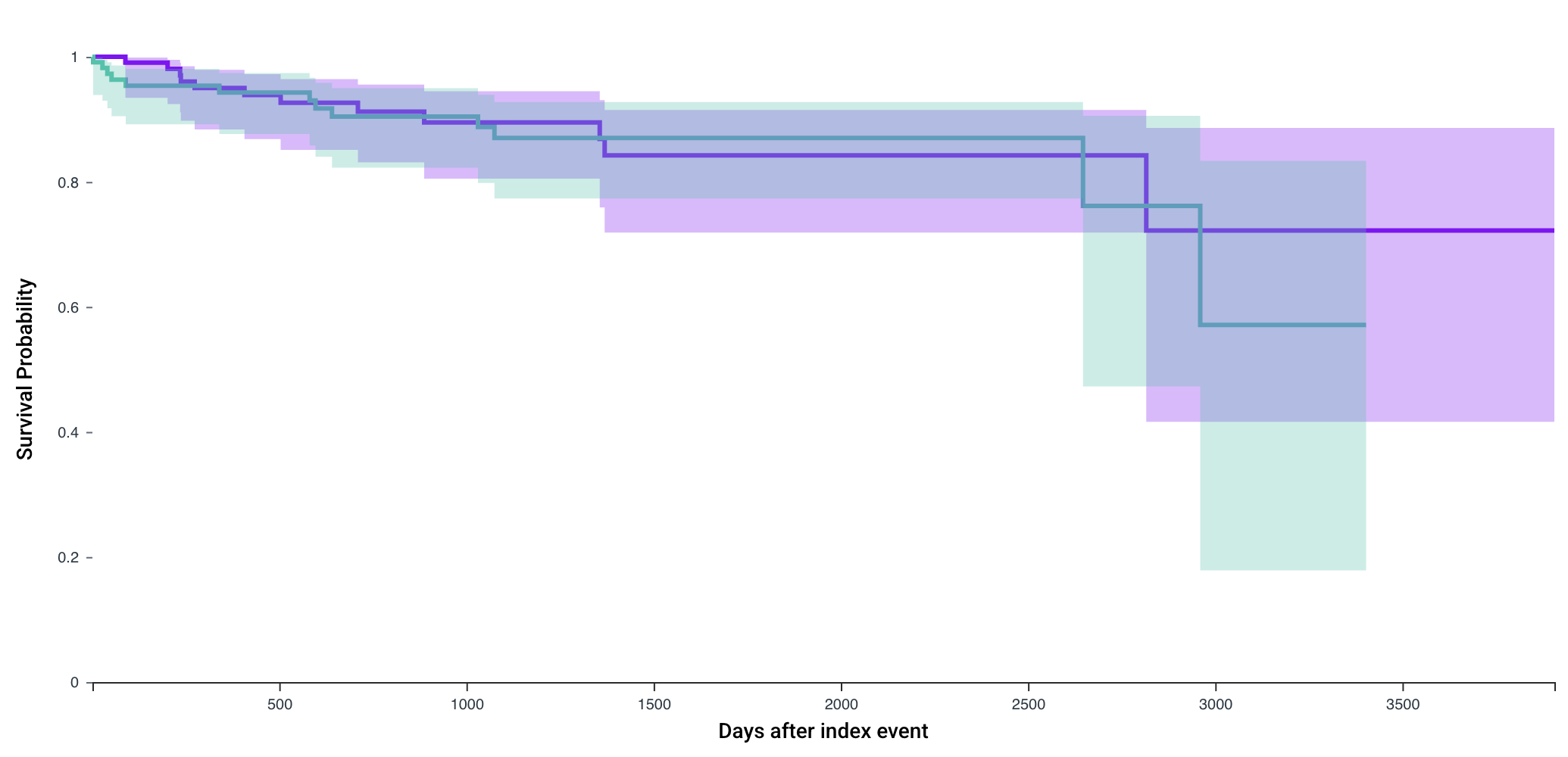
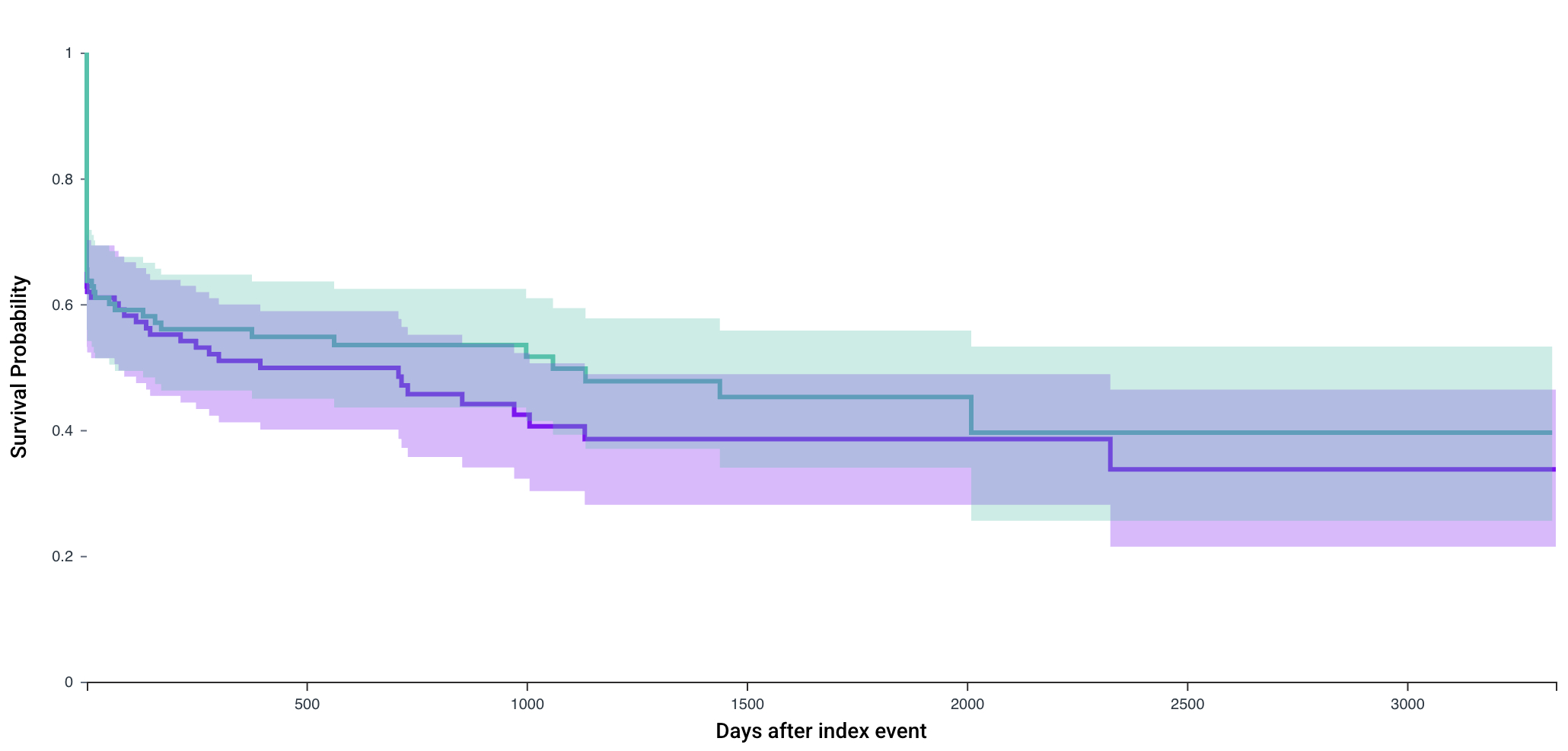
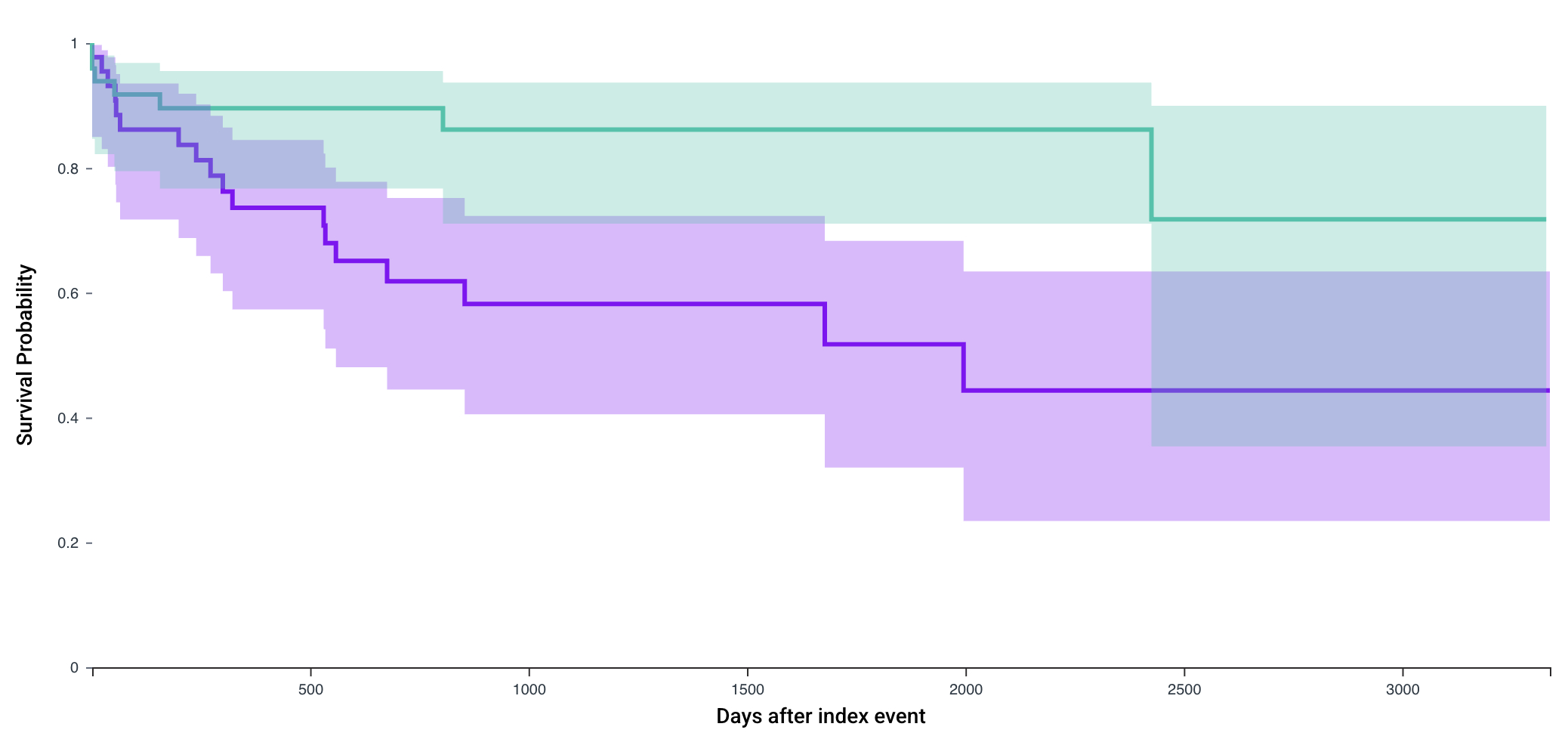
Following propensity score matching, mortality was similar between cohorts: 10.6% (12/113) in the ICD group vs. 11.5% (13/113) in the PPM group (risk difference -0.009%, 95% CI: -0.09-0.07, p =0.83; HR: 0.93, 95% CI: 0.42-2.03, p=0.91). The rates of hospitalization were similar as well: 55.6% (63/113) in ICD group vs. 29.6% (56/113) in the PPM group (risk difference 0.06%, 95% CI: -0.07-0.19, p= 0.35; HR: 1.14, p=0.56). However, the rates of heart failure diagnosis post-device implantation was greater in ICD group (40.9%, 18/44) vs. PPM group (20.4%, 10/49, risk difference: 0.21, 95% CI: 0.02-0.39, p=0.03).
Conclusion:
In CS patients with preserved LVEF, ICD implantation did not improve mortality or hospitalization rates compared to PPM. However, incident HF was significantly more frequent in the ICD group, potentially reflecting unmeasured confounding factors influencing device selection. These findings underscore the need for prospective studies to better inform device choice in this complex population.
Patients with cardiac sarcoidosis (CS) generally have a poor prognosis, due to an increased risk for arrhythmias, heart failure (HF), and sudden cardiac death often necessitating device therapy. However, in patients with preserved left ventricular ejection fraction (LVEF), the optimal device—implantable cardioverter-defibrillator (ICD) vs. permanent pacemaker (PPM)—remains unclear. Our study assessed the impact of ICD vs. PPM in CS on clinical outcomes, including mortality, hospitalization, and HF development in this population.
Objective:
Evaluate mortality, hospitalization, and development of HF in patients with CS and normal LVEF who received an ICD vs PPM.
Methods:
We conducted a retrospective cohort analysis using the TriNetX Research Network, which aggregates electronic health records from 102 healthcare organizations. Adult patients (≥18 years) with CS and a LVEF > 35% receiving either an ICD (n=1,403) or PPM (n=115) after initial diagnosis were included. Patients with reduced LVEF and prior ventricular tachycardia were excluded. Propensity score matching (1:1) was used to adjust for baseline differences across 12 demographic, clinical, and laboratory variables (n = 113 in each group). The primary outcomes were all-cause mortality, hospitalizations, and incidence of HF following device implantation. Risk ratios, Kaplan-Meier survival analysis, hazard ratios, and p-values were used for comparative analysis.
Results:
Following propensity score matching, mortality was similar between cohorts: 10.6% (12/113) in the ICD group vs. 11.5% (13/113) in the PPM group (risk difference -0.009%, 95% CI: -0.09-0.07, p =0.83; HR: 0.93, 95% CI: 0.42-2.03, p=0.91). The rates of hospitalization were similar as well: 55.6% (63/113) in ICD group vs. 29.6% (56/113) in the PPM group (risk difference 0.06%, 95% CI: -0.07-0.19, p= 0.35; HR: 1.14, p=0.56). However, the rates of heart failure diagnosis post-device implantation was greater in ICD group (40.9%, 18/44) vs. PPM group (20.4%, 10/49, risk difference: 0.21, 95% CI: 0.02-0.39, p=0.03).
Conclusion:
In CS patients with preserved LVEF, ICD implantation did not improve mortality or hospitalization rates compared to PPM. However, incident HF was significantly more frequent in the ICD group, potentially reflecting unmeasured confounding factors influencing device selection. These findings underscore the need for prospective studies to better inform device choice in this complex population.
More abstracts on this topic:
Constrictive Pericarditis Due to Sarcoidosis: Role of Multimodality Imaging in a Patient with a Metal Jacket Full of Calcification
Syed Alveena, Motairek Issam, El Hajjar Abdel Hadi, Abdulhai Farah, Saraswati Ushasi, Safdar Ahmad, Bhalla Jaideep Singh, Wang Tom Kai Ming, Ramchand Jay, Klein Allan
All-cause mortality for Patients with Preserved Ejection Fraction Heart Failure stratified by B-blocker Therapy and Presence of Permanent Pacemaker.Leavitt Jonas, Cunn Gregory, Coleman Kristie, Ahmad Sana, Bekiaridou Alexandra, Gasparis Christopher, Fishbein Joanna, Mountantonakis Stavros