Final ID: Mo1035
Evaluating Procedural Safety and Outcomes In GLP-1 Exposed Patients Undergoing TEE
Abstract Body (Do not enter title and authors here):
Background:
Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) like semaglutide and liraglutide are commonly used for type 2 diabetes, weight loss, and cardiovascular risk reduction. However, their effect on gastric emptying has raised concern for aspiration risk during sedated procedures. While current anesthesia guidelines recommend holding GLP-1 RAs before elective procedures, there's limited data specific to TEE. This study evaluates the risk of aspiration and other post-procedural events in patients on GLP-1 RAs undergoing TEE procedure.
Methods:
We conducted a retrospective cohort study of patients ≥18 years old who underwent TEE between January 1, 2016, and April 1, 2025. The primary cohort included 9,668 patients with diabetes on GLP-1 therapy for at least 6 months prior to TEE, and propensity score matched (PSM) 1:1 to controls not on GLP-1s. A secondary analysis evaluated 777 patients on GLP-1 RAs and without diabetes. Patients with known gastroparesis, abdominal surgery, neurologic conditions, chronic opioid use, small bowel obstruction, ileus, or respiratory failure prior to TEE were excluded. The primary outcome was aspiration pneumonia within 30 days. Secondary outcomes included acute hypoxemic respiratory failure (AHRF), myocardial infarction (MI), and atrial fibrillation (AFib).
Results:
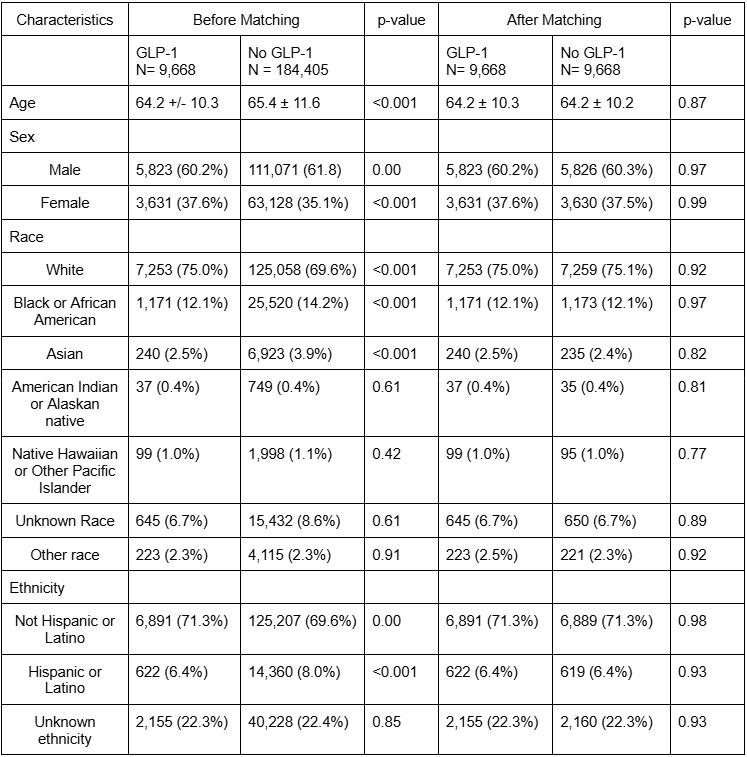
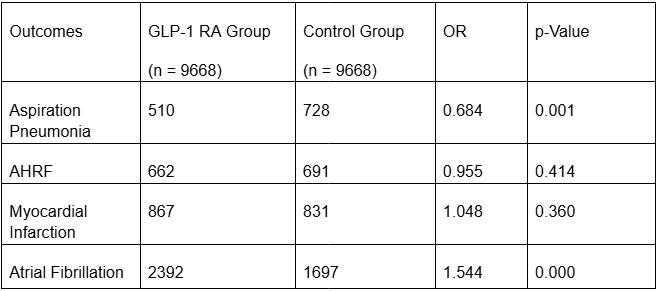
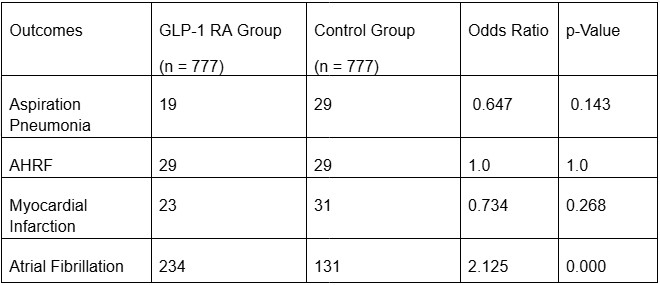
A total of 332,037 adult patients with diabetes who underwent TEE (inpatient and outpatient) were identified, of whom 9,668 were prescribed GLP-1RA. Those that met the criteria were divided into 2 cohorts based on GLP-1RA use. Before PSM, GLP-1RA users were younger (64.2 +/- 10.3 vs 65.2 +/- 11.6), predominantly males (60.2% vs 37.6%) and white (75%) (Table 1). After PSM, all demographic characteristics between the GLP-1RA users and non-GLP-1RA cohorts were well-balanced, with no statistically significant differences. Aspiration pneumonia occurred less frequently in those on GLP-1s (5.3% vs. 7.5%, OR 0.684, p<0.001). No significant differences were observed in AHRF (6.8% vs. 7.1%, p=0.414), and MI (9.0% vs. 8.6%, p=0.360). AFib remained significant between the two cohorts (24.7% vs. 17.6%, OR 1.544, p<0.001) (Table 2). In a subgroup analysis, whereby diabetics were excluded, similar outcomes were observed (Table 3).
Conclusion:
In patients undergoing TEE, GLP-1 RA use was associated with similar or lower rates of aspiration pneumonia but a higher incidence of AFib, regardless of diabetes status. Prospective studies are needed to confirm these findings.
Background:
Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) like semaglutide and liraglutide are commonly used for type 2 diabetes, weight loss, and cardiovascular risk reduction. However, their effect on gastric emptying has raised concern for aspiration risk during sedated procedures. While current anesthesia guidelines recommend holding GLP-1 RAs before elective procedures, there's limited data specific to TEE. This study evaluates the risk of aspiration and other post-procedural events in patients on GLP-1 RAs undergoing TEE procedure.
Methods:
We conducted a retrospective cohort study of patients ≥18 years old who underwent TEE between January 1, 2016, and April 1, 2025. The primary cohort included 9,668 patients with diabetes on GLP-1 therapy for at least 6 months prior to TEE, and propensity score matched (PSM) 1:1 to controls not on GLP-1s. A secondary analysis evaluated 777 patients on GLP-1 RAs and without diabetes. Patients with known gastroparesis, abdominal surgery, neurologic conditions, chronic opioid use, small bowel obstruction, ileus, or respiratory failure prior to TEE were excluded. The primary outcome was aspiration pneumonia within 30 days. Secondary outcomes included acute hypoxemic respiratory failure (AHRF), myocardial infarction (MI), and atrial fibrillation (AFib).
Results:
A total of 332,037 adult patients with diabetes who underwent TEE (inpatient and outpatient) were identified, of whom 9,668 were prescribed GLP-1RA. Those that met the criteria were divided into 2 cohorts based on GLP-1RA use. Before PSM, GLP-1RA users were younger (64.2 +/- 10.3 vs 65.2 +/- 11.6), predominantly males (60.2% vs 37.6%) and white (75%) (Table 1). After PSM, all demographic characteristics between the GLP-1RA users and non-GLP-1RA cohorts were well-balanced, with no statistically significant differences. Aspiration pneumonia occurred less frequently in those on GLP-1s (5.3% vs. 7.5%, OR 0.684, p<0.001). No significant differences were observed in AHRF (6.8% vs. 7.1%, p=0.414), and MI (9.0% vs. 8.6%, p=0.360). AFib remained significant between the two cohorts (24.7% vs. 17.6%, OR 1.544, p<0.001) (Table 2). In a subgroup analysis, whereby diabetics were excluded, similar outcomes were observed (Table 3).
Conclusion:
In patients undergoing TEE, GLP-1 RA use was associated with similar or lower rates of aspiration pneumonia but a higher incidence of AFib, regardless of diabetes status. Prospective studies are needed to confirm these findings.
More abstracts on this topic:
Chronotherapy in Hypertension: A Meta-Analysis of the Cardiovascular Effects of Bedtime Versus Morning Antihypertensive Administration
Lee Yebon, Riaz Minahil, Ajaz Hareem, Muhammad Daniyal Shaikh, Fahim Syeda, Aftab Zunaira, Tauiqr Habiba, Ashraf Danish Ali, Sarwar Mahwish, Noor Amna, Batool Fizza, Murad Khatoon Naveen
Optimizing AV Nodal Ablation: The Role of Coronary Dominance in Procedural PlanningMazumder Samia, Madanat Luai, Kheyrbek Mazhed, Foglesong Adam, Bloomingdale Richard, Kutinsky Ilana