Final ID: MP234
Longitudinal Analysis of Mild Cognitive Impairment and Dementia in Heart Failure
Abstract Body (Do not enter title and authors here): Introduction: Heart failure (HF) is associated with higher risk of developing cognitive impairment including mild cognitive impairment (MCI) and dementia. However, longitudinal changes in cognitive status in HF are less understood.
Research questions: What percent of participants with HF have MCI or dementia at baseline using a rigorous diagnostic consensus? What percent develop MCI or dementia 16-36 months after baseline?
Methods: A longitudinal descriptive study was conducted using supplement study data from a 3-arm randomized controlled trial. In the parent study, an 8-week cognitive training intervention (BrainHQ) was tested for efficacy compared with computerized crossword puzzles and usual care control conditions. There was no significant improvement in memory over 8 months of follow-up. Of 256 participants with HF (MoCA ≥ 19) randomized in the parent study, 144 were eligible and invited for the supplement study, and 96 consented. The supplement study added one additional follow-up interview between 16 and 36 months after baseline to assess long-term BrainHQ efficacy.
Cognitive status (normal, MCI, or dementia) was determined by diagnostic consensus among a group of experts from neurology, neuropsychology, cardiology, and nursing who reviewed cognitive test scores, medical history, and supporting data (e.g., instrumental activities of daily living, depressive symptoms). A 100% consensus was reached for all 96 participants.
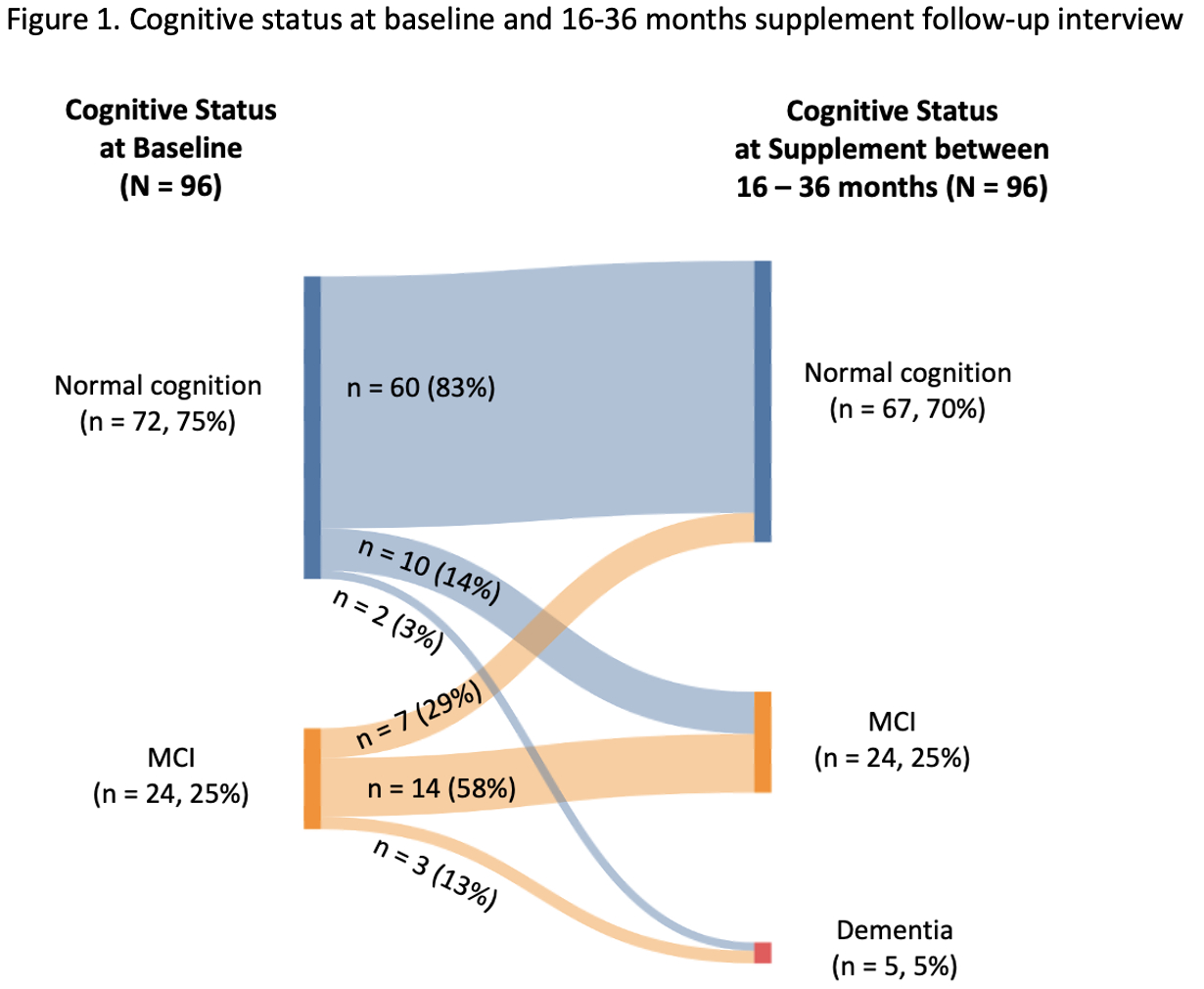
Results: The sample was 51% women, mean age 65 ± 12 years. At baseline, 72 of 96 participants (75%) had normal cognition and 24 (25%) had MCI (Figure 1): 5 amnestic MCI , 15 non-amnestic MCI, and 4 multi-domain MCI.
At the supplement follow-up, 74 (77%) retained their baseline cognitive status, 10 (11%) developed MCI, 5 (5%) developed dementia, and 7 (7%) converted from MCI to normal cognition. Of 72 with baseline normal cognition, 60 (83%) remained normal, 10 (14%) developed MCI, and 2 (3%) developed dementia. Of 24 with baseline MCI, 14 (58%) remained MCI, 3 (13%) developed dementia, and 7 (29%) improved to normal cognition.
Conclusion: Using diagnostic consensus, MCI was identified among 25% of participants at baseline. Sixteen percent developed MCI or dementia at the follow-up. Notably, 29% of participants with baseline MCI improved to normal cognition at the follow-up. These findings highlight the need for interventions to identify, delay or reverse cognitive decline in HF.
Research questions: What percent of participants with HF have MCI or dementia at baseline using a rigorous diagnostic consensus? What percent develop MCI or dementia 16-36 months after baseline?
Methods: A longitudinal descriptive study was conducted using supplement study data from a 3-arm randomized controlled trial. In the parent study, an 8-week cognitive training intervention (BrainHQ) was tested for efficacy compared with computerized crossword puzzles and usual care control conditions. There was no significant improvement in memory over 8 months of follow-up. Of 256 participants with HF (MoCA ≥ 19) randomized in the parent study, 144 were eligible and invited for the supplement study, and 96 consented. The supplement study added one additional follow-up interview between 16 and 36 months after baseline to assess long-term BrainHQ efficacy.
Cognitive status (normal, MCI, or dementia) was determined by diagnostic consensus among a group of experts from neurology, neuropsychology, cardiology, and nursing who reviewed cognitive test scores, medical history, and supporting data (e.g., instrumental activities of daily living, depressive symptoms). A 100% consensus was reached for all 96 participants.
Results: The sample was 51% women, mean age 65 ± 12 years. At baseline, 72 of 96 participants (75%) had normal cognition and 24 (25%) had MCI (Figure 1): 5 amnestic MCI , 15 non-amnestic MCI, and 4 multi-domain MCI.
At the supplement follow-up, 74 (77%) retained their baseline cognitive status, 10 (11%) developed MCI, 5 (5%) developed dementia, and 7 (7%) converted from MCI to normal cognition. Of 72 with baseline normal cognition, 60 (83%) remained normal, 10 (14%) developed MCI, and 2 (3%) developed dementia. Of 24 with baseline MCI, 14 (58%) remained MCI, 3 (13%) developed dementia, and 7 (29%) improved to normal cognition.
Conclusion: Using diagnostic consensus, MCI was identified among 25% of participants at baseline. Sixteen percent developed MCI or dementia at the follow-up. Notably, 29% of participants with baseline MCI improved to normal cognition at the follow-up. These findings highlight the need for interventions to identify, delay or reverse cognitive decline in HF.
More abstracts on this topic:
Association Between Kidney Function and Severity of White Matter Hyperintensity: The Atherosclerosis Risk in Communities Study
Littig Lauren, Krothapalli Neeharika, Wong Ka-ho, Kim Yvonne, Smith Harper, De Havenon Adam
Age and White Matter Injury due to Cerebral Small Vessel Disease are Synergistically Associated with Impaired Neurovascular Coupling.Yang Sheng, Webb Alastair