Final ID: MP111
Sex and Racial Disparities in Atherosclerotic Heart Disease Mortality Among Older Adults in the United States: A CDC WONDER Database Analysis (1999–2020)
Abstract Body (Do not enter title and authors here): Background: Atherosclerotic heart disease (ASHD) remains a leading cause of death among older adults in the United States. However, disparities in ASHD-related mortality by sex and race remain underexplored.
Research Question: This study evaluates temporal trends and demographic disparities in ASHD mortality among individuals aged 65 years and older using national death certificate data from CDC Wonder.
Methods: Mortality data from CDC WONDER database was analyzed, identifying ASHD-related deaths using ICD-10 code I25.1. ASHD was listed as a contributing or underlying cause of death. Age-adjusted mortality rates (AAMRs) per 100,000 were calculated and stratified by sex
and race. Joinpoint regression was used to estimate Annual Percent Change (APC) and Average Annual Percent Change (AAPC), identifying significant shifts in trend over the study period.
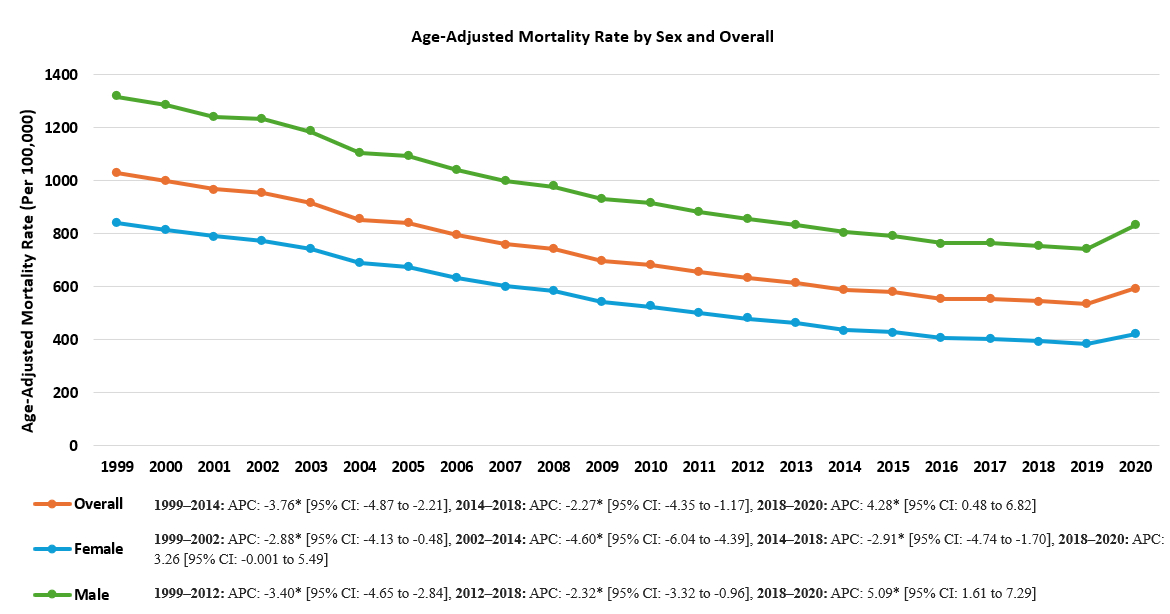
Results: From 1999 to 2020, ASHD accounted for 6,571,263 deaths in the study population. Overall, AAMRs declined significantly from 1999 to 2014 (APC: −3.7695% CI: -4.87 to -2.21), with a continued but slower decline from 2014 to 2018 (APC: −2.27%, 95% CI: -4.35 to -1.17),
followed by a significant increase from 2018 to 2020 (APC: +4.28%, 95% CI: 0.48 to 6.82). Males consistently exhibited higher AAMRs than females (942.51 vs 555.21, respectively). Among males, mortality declined through 2018 (APCs: −3.40%, 95% CI: -4.65 to -2.84, and
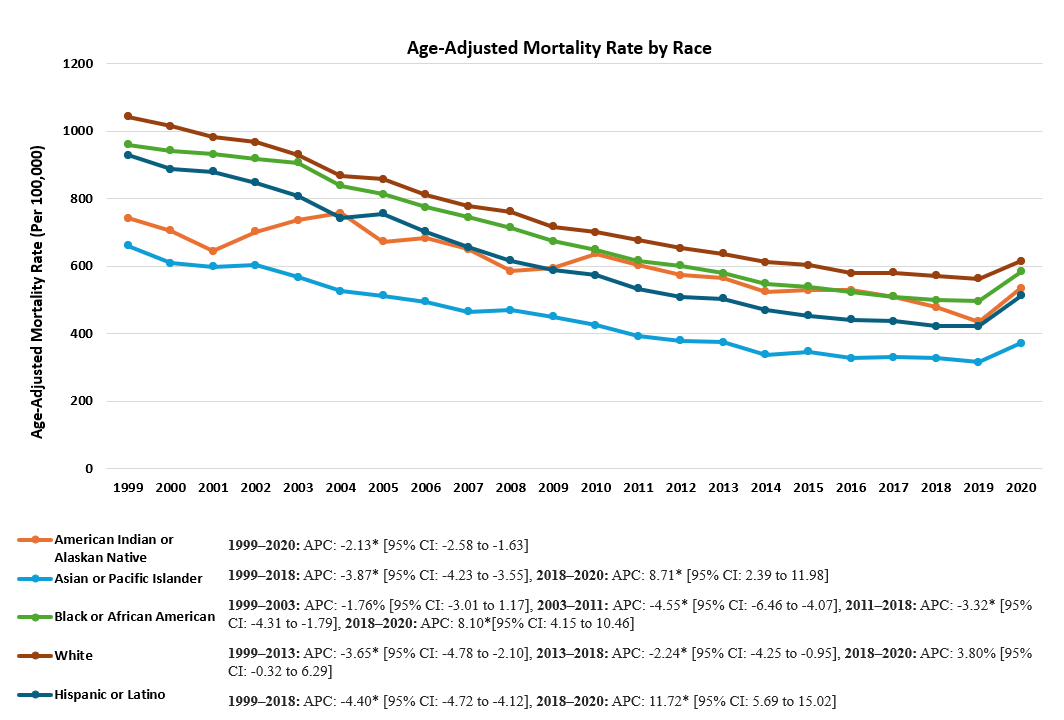
−2.31%, 95% CI: -3.32 to -0.96), then rose from 2018 to 2020 (APC: 5.09%, 95% CI: 1.61 to 7.29), with an overall AAPC of -2.31(95% CI: -2.56 to -2.15). Females showed a steady decline with a potential upward shift beginning in 2018 (APC: 3.26%, 95% CI: -0.001 to 5.49), and an overall AAPC of -3.31 (95% CI: -3.54 to -3.12). Racial disparities persisted throughout. Whites had the highest AAMRs (737.03), while Non-Hispanic Asians had the lowest (409.90). All racial groups experienced declining mortality trends through 2018, followed by increases through 2020—except American Indians, whose AAMRs continued to decline (APC: −2.13%, 95% CI: -2.58 to -1.63).
Conclusion: While ASHD mortality declined among older adults for nearly two decades, the recent upward trend—particularly among males and most racial groups—signals a concerning reversal. Persisting racial disparities and sex-based differences highlight the urgent need for equity-driven cardiovascular prevention and intervention strategies tailored to the aging U.S. population.
Research Question: This study evaluates temporal trends and demographic disparities in ASHD mortality among individuals aged 65 years and older using national death certificate data from CDC Wonder.
Methods: Mortality data from CDC WONDER database was analyzed, identifying ASHD-related deaths using ICD-10 code I25.1. ASHD was listed as a contributing or underlying cause of death. Age-adjusted mortality rates (AAMRs) per 100,000 were calculated and stratified by sex
and race. Joinpoint regression was used to estimate Annual Percent Change (APC) and Average Annual Percent Change (AAPC), identifying significant shifts in trend over the study period.
Results: From 1999 to 2020, ASHD accounted for 6,571,263 deaths in the study population. Overall, AAMRs declined significantly from 1999 to 2014 (APC: −3.7695% CI: -4.87 to -2.21), with a continued but slower decline from 2014 to 2018 (APC: −2.27%, 95% CI: -4.35 to -1.17),
followed by a significant increase from 2018 to 2020 (APC: +4.28%, 95% CI: 0.48 to 6.82). Males consistently exhibited higher AAMRs than females (942.51 vs 555.21, respectively). Among males, mortality declined through 2018 (APCs: −3.40%, 95% CI: -4.65 to -2.84, and
−2.31%, 95% CI: -3.32 to -0.96), then rose from 2018 to 2020 (APC: 5.09%, 95% CI: 1.61 to 7.29), with an overall AAPC of -2.31(95% CI: -2.56 to -2.15). Females showed a steady decline with a potential upward shift beginning in 2018 (APC: 3.26%, 95% CI: -0.001 to 5.49), and an overall AAPC of -3.31 (95% CI: -3.54 to -3.12). Racial disparities persisted throughout. Whites had the highest AAMRs (737.03), while Non-Hispanic Asians had the lowest (409.90). All racial groups experienced declining mortality trends through 2018, followed by increases through 2020—except American Indians, whose AAMRs continued to decline (APC: −2.13%, 95% CI: -2.58 to -1.63).
Conclusion: While ASHD mortality declined among older adults for nearly two decades, the recent upward trend—particularly among males and most racial groups—signals a concerning reversal. Persisting racial disparities and sex-based differences highlight the urgent need for equity-driven cardiovascular prevention and intervention strategies tailored to the aging U.S. population.
More abstracts on this topic:
Accumulation of Epicardial Adipose Tissue as a Marker of Diastolic Dysfunction in Patients With Preserved Left Ventricular Ejection Fraction Undergoing Coronary Computed Tomography Angiograph
Ishikawa Hirotoshi, Kasayuki Noriaki, Fukuda Daiju, Otsuka Kenichiro, Sugiyama Takatoshi, Yamaura Hiroki, Hojo Kana, Kawa Yoshinori, Shintani Ako, Ito Asahiro, Yamazaki Takanori
A Case of Transient Cortical Blindness occurring during Percutaneous Transluminal Coronary Angiography for Acute Coronary Syndrome.Adelakun Adeniyi, Farouji Iyad, Haddad Ahmad, Szwed Stanley