Final ID: MP851
Dual Risk of Bleeding and Thrombosis in Thrombophilia Patients Undergoing Transcatheter Edge-to-Edge Mitral Valve Repair: A Multicenter Real-World Analysis
Abstract Body (Do not enter title and authors here):
Background:
Patients with thrombophilia undergoing transcatheter edge-to-edge mitral valve repair (M-TEER) represent a clinical challenge due to elevated risks of both thrombotic and bleeding events. Optimal antithrombotic management in this population remains undefined.
Methods:
We conducted a multicenter, retrospective cohort study using the TriNetX Global Collaborative Network, incorporating electronic health records from 144 healthcare organizations. Adults (≥18 years) who underwent M-TEER were categorized into two cohorts: those with major thrombophilia (n=342) and those without any thrombophilia (n=6,857). Patients with prior major cardiac surgery were excluded. Propensity score matching was performed to balance baseline characteristics. Outcomes included major bleeding, venous thromboembolism (VTE), ischemic stroke, arterial thromboembolism, and all-cause mortality, analyzed using risk ratios and Kaplan–Meier survival estimates.
Results:
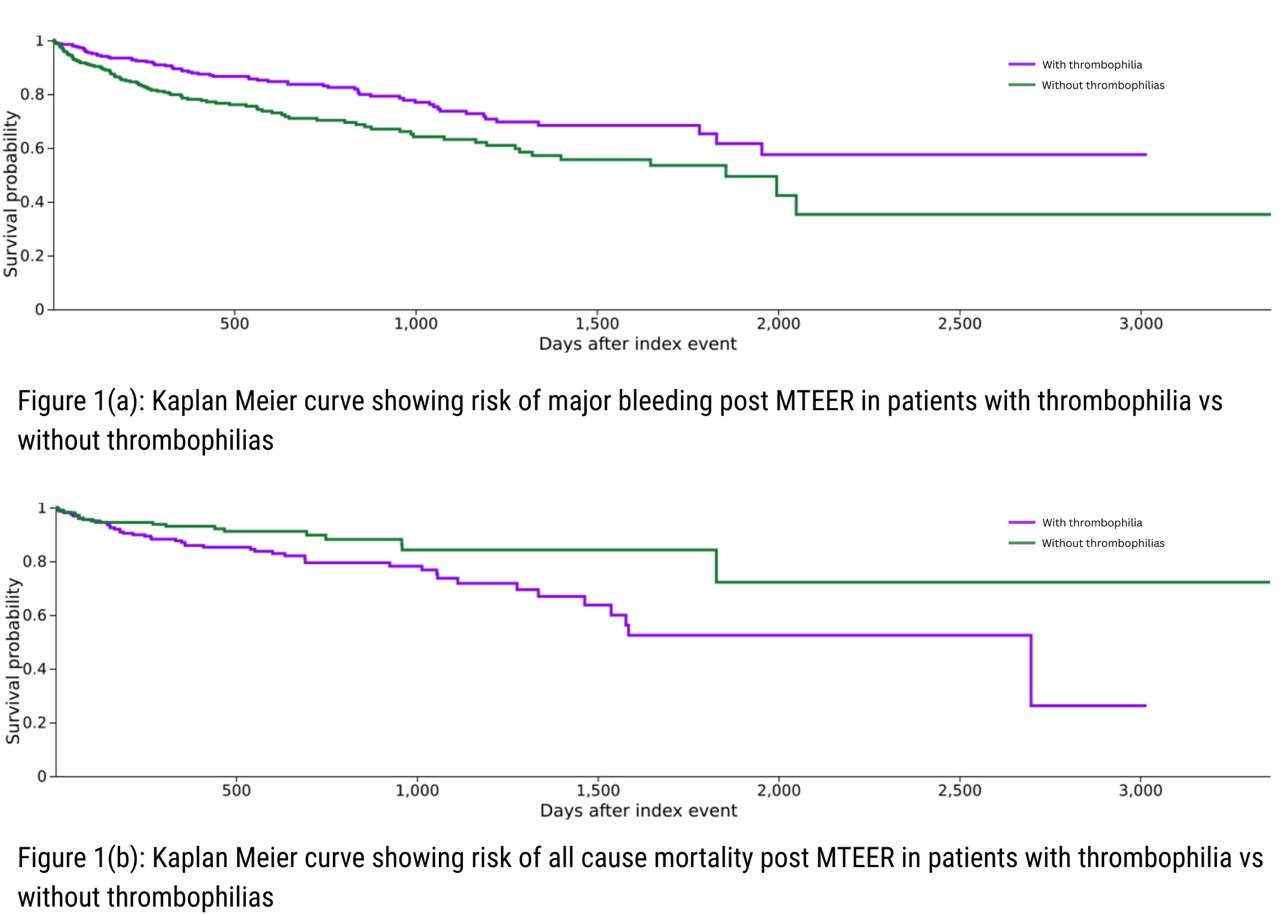
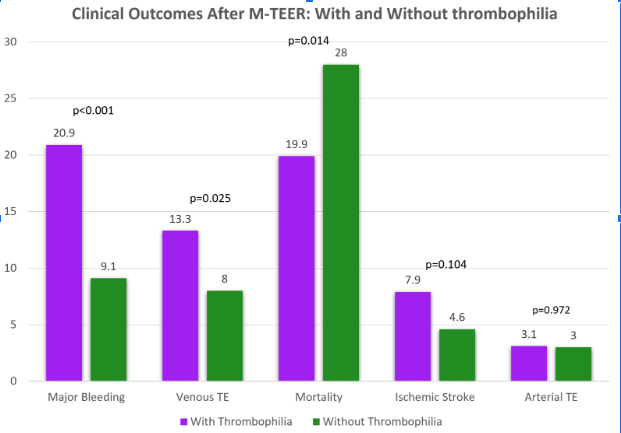
After 1:1 matching, 678 patients were analyzed (thrombophilia: n=339; control: n=339). Thrombophilia patients had significantly higher rates of major bleeding (20.9% vs. 9.1%, p < 0.001; RR, 2.30 [95% CI, 1.41–3.74]) and VTE (13.3% vs. 8.0%, p = 0.025; RR, 1.67 [1.06–2.62]). Rates of ischemic stroke (7.9% vs. 4.6%, p=0.104) and arterial thromboembolism (3.1% vs. 3.0%, p=0.972) were not significantly different. Despite this, all-cause mortality was lower in the thrombophilia group (19.9% vs. 28.0%, p=0.014; RR 0.71 [0.54–0.94]). Kaplan–Meier curves also showed that thrombophilia patients had significantly lower all-cause mortality (HR: 0.579, 95% CI: 0.423–0.793; p = 0.001) but higher bleeding risk (HR: 2.020, 95% CI: 1.198–3.406; p = 0.007) compared to those without thrombophilia. The absence of granular anticoagulation data (e.g., INR, PT, APTT) limited assessment of therapeutic intensity.
Conclusions:
Thrombophilia confers a dual risk of bleeding and thrombotic events in patients undergoing M-TEER, emphasizing the need for individualized antithrombotic strategies and vigilant monitoring. Despite intensive anticoagulation, VTE risk remains elevated. Paradoxically lower mortality in the thrombophilia cohort may reflect more intensive clinical surveillance, selection bias, or residual confounding. Increased bleeding risk may be due to intensified antithrombotic regimens, while the elevated VTE risk likely reflects the inherent prothrombotic state. Prospective studies are needed to optimize outcomes in this high-risk group.
Background:
Patients with thrombophilia undergoing transcatheter edge-to-edge mitral valve repair (M-TEER) represent a clinical challenge due to elevated risks of both thrombotic and bleeding events. Optimal antithrombotic management in this population remains undefined.
Methods:
We conducted a multicenter, retrospective cohort study using the TriNetX Global Collaborative Network, incorporating electronic health records from 144 healthcare organizations. Adults (≥18 years) who underwent M-TEER were categorized into two cohorts: those with major thrombophilia (n=342) and those without any thrombophilia (n=6,857). Patients with prior major cardiac surgery were excluded. Propensity score matching was performed to balance baseline characteristics. Outcomes included major bleeding, venous thromboembolism (VTE), ischemic stroke, arterial thromboembolism, and all-cause mortality, analyzed using risk ratios and Kaplan–Meier survival estimates.
Results:
After 1:1 matching, 678 patients were analyzed (thrombophilia: n=339; control: n=339). Thrombophilia patients had significantly higher rates of major bleeding (20.9% vs. 9.1%, p < 0.001; RR, 2.30 [95% CI, 1.41–3.74]) and VTE (13.3% vs. 8.0%, p = 0.025; RR, 1.67 [1.06–2.62]). Rates of ischemic stroke (7.9% vs. 4.6%, p=0.104) and arterial thromboembolism (3.1% vs. 3.0%, p=0.972) were not significantly different. Despite this, all-cause mortality was lower in the thrombophilia group (19.9% vs. 28.0%, p=0.014; RR 0.71 [0.54–0.94]). Kaplan–Meier curves also showed that thrombophilia patients had significantly lower all-cause mortality (HR: 0.579, 95% CI: 0.423–0.793; p = 0.001) but higher bleeding risk (HR: 2.020, 95% CI: 1.198–3.406; p = 0.007) compared to those without thrombophilia. The absence of granular anticoagulation data (e.g., INR, PT, APTT) limited assessment of therapeutic intensity.
Conclusions:
Thrombophilia confers a dual risk of bleeding and thrombotic events in patients undergoing M-TEER, emphasizing the need for individualized antithrombotic strategies and vigilant monitoring. Despite intensive anticoagulation, VTE risk remains elevated. Paradoxically lower mortality in the thrombophilia cohort may reflect more intensive clinical surveillance, selection bias, or residual confounding. Increased bleeding risk may be due to intensified antithrombotic regimens, while the elevated VTE risk likely reflects the inherent prothrombotic state. Prospective studies are needed to optimize outcomes in this high-risk group.
More abstracts on this topic:
A Rare Case of Loeffler Endocarditis and Intracardiac Thrombus in the setting of FIP1L1-PDGFRA Mutation
Shaik Aleesha, Pankayatselvan Varayini, Mazar Michael, Bokhoor Pooya
Baseline Characteristics and Outcomes of Barlow Syndrome Patients with and without Atrial FibrillationRoma Nicholas, Desai Spandan, Cohen Brett, Pattoli Megan, Miller Luke, Durkin Michael