Final ID: Sa3014
Maternal Vascular Endothelial Growth Factor Signaling and Hospital Length of Stay Association in Hypoplastic Left Heart Syndrome Post Stage One Palliation
Abstract Body (Do not enter title and authors here): Background: Neonates with critical congenital heart disease (CHD) have significant variability in outcomes not explained by traditional risk factors. Previous work showed that pregnancies with CHD have placental abnormalities likely related to abnormal vascular signaling. Variability in vascular signaling may identify neonates with increased risk for adverse outcomes. Our objective was to identify differences in maternal-fetal biomarkers and their associations with outcomes post-cardiac surgery.
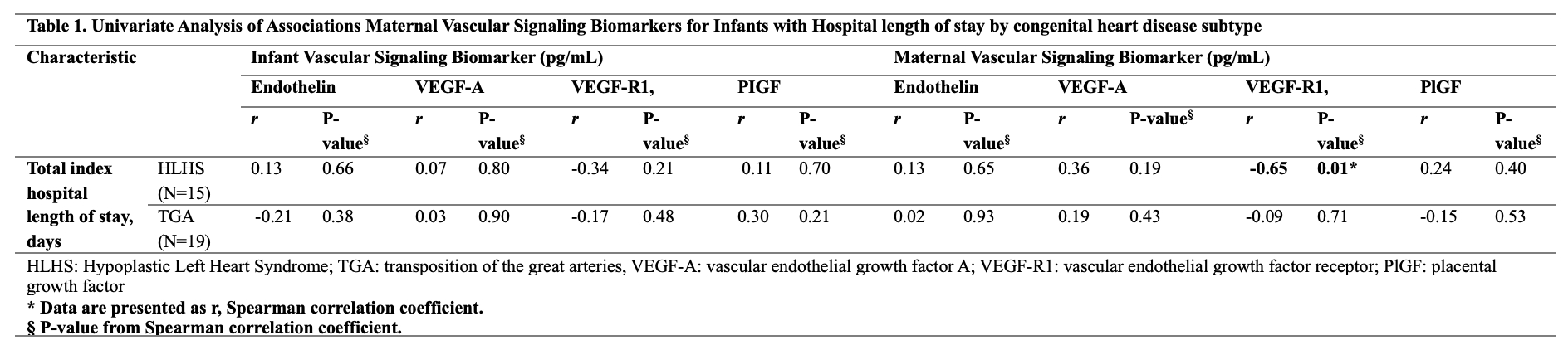
Methods: We examined the balance of proangiogenic (vascular endothelial growth factor A VEGF-A and placental growth factor PLGF) and anti-angiogenic (endothelin, vascular endothelial growth factor receptor VEGF-R) biomarkers in mother/infant dyads. We included Hypoplastic left Heart Syndrome (HLHS) and d-Transposition of the Great Arteries (TGA). Blood samples were collected from the mothers within 24h post-delivery and from cord venous blood. We included women 18-40 years of age with single gestation delivered at 36+ weeks. Excluded were infants with genetic syndromes, mothers with diabetes, smoking history, or substance use disorder. Data also included infant demographics, gestational age, age at surgery, birth weight, index surgery with bypass time, deep hypothermic circulatory arrest (DHCA) duration, use of antegrade cerebral perfusion (ACP), duration of cross-clamp, post-operative complications, and hospital length of stay (LOS). Spearman correlation coefficient (r ) was used to assess associations of fetal and maternal markers with LOS.
Results: TGA group (N=19) was more likely to have longer cross-clamp times (p=0.002). HLHS group (N=15) was more likely to have had DHCA and ACP, to have a longer LOS, and to return with an open chest (p<0.003). In the combined cohort (N=34), lower maternal VEGF-R levels were associated with return with an open-chest and another bypass during admission (p=0.04). In HLHS, maternal VEGF-R levels were inversely correlated with LOS (r = -0.65, p=0.01). No fetal markers were associated with LOS outcomes in either group.
Conclusion: Maternal VEGF-R levels and not neonatal biomarkers were associated with some post-operative outcomes, with maternal VEGF-R inversely related to LOS in HLHS and directly related to a more complex post-op course in the combined group. This further emphasizes the importance of maternal-fetal interactions and underscores the need to better define the role of vascular signaling in CHD and post-op outcomes
Methods: We examined the balance of proangiogenic (vascular endothelial growth factor A VEGF-A and placental growth factor PLGF) and anti-angiogenic (endothelin, vascular endothelial growth factor receptor VEGF-R) biomarkers in mother/infant dyads. We included Hypoplastic left Heart Syndrome (HLHS) and d-Transposition of the Great Arteries (TGA). Blood samples were collected from the mothers within 24h post-delivery and from cord venous blood. We included women 18-40 years of age with single gestation delivered at 36+ weeks. Excluded were infants with genetic syndromes, mothers with diabetes, smoking history, or substance use disorder. Data also included infant demographics, gestational age, age at surgery, birth weight, index surgery with bypass time, deep hypothermic circulatory arrest (DHCA) duration, use of antegrade cerebral perfusion (ACP), duration of cross-clamp, post-operative complications, and hospital length of stay (LOS). Spearman correlation coefficient (r ) was used to assess associations of fetal and maternal markers with LOS.
Results: TGA group (N=19) was more likely to have longer cross-clamp times (p=0.002). HLHS group (N=15) was more likely to have had DHCA and ACP, to have a longer LOS, and to return with an open chest (p<0.003). In the combined cohort (N=34), lower maternal VEGF-R levels were associated with return with an open-chest and another bypass during admission (p=0.04). In HLHS, maternal VEGF-R levels were inversely correlated with LOS (r = -0.65, p=0.01). No fetal markers were associated with LOS outcomes in either group.
Conclusion: Maternal VEGF-R levels and not neonatal biomarkers were associated with some post-operative outcomes, with maternal VEGF-R inversely related to LOS in HLHS and directly related to a more complex post-op course in the combined group. This further emphasizes the importance of maternal-fetal interactions and underscores the need to better define the role of vascular signaling in CHD and post-op outcomes
More abstracts on this topic:
Mechanical Circulatory Support in Pregnancy
Goodwin Ashley, Wendl Elizabeth, Jones Tara
Aortic Stenosis in Pregnancy: A Multidisciplinary Team ApproachCaplan Alex, Jackson Jordan, Kalot Mohamad, Yost Gregory