Final ID: MP2434
Impact of Area Deprivation Index on Gaps in Care for Young Adults with Congenital Heart Disease
Abstract Body (Do not enter title and authors here): Introduction: Neighborhood socioeconomic deprivation has been previously linked with inferior health outcomes such as mortality and hospitalizations for adults with congenital heart disease (CHD). However, little is known about its impact on receiving guideline recommended ACHD care for adults especially as they transition from pediatric to adult health system.
Objective: To evaluate the effect of neighborhood socioeconomic deprivation on gaps in adult CHD specialist visits for young adults with CHD
Methods: We conducted a retrospective observational study using electronic health record data from University of California, San Francisco. Our inclusion criteria were patients aged 18-40 who had at least one encounter between 2018 and 2022. The independent variable was neighborhood socioeconomic deprivation measured by the area deprivation index (ADI), a composite index of census-derived indicators. Patients with ADI score of 1-2 were considered least deprived, those with 3-5 as moderately deprived, and those 7-10 as most deprived. The primary outcome was gaps in any ACHD specialist visit during the study period. Secondary outcome was gaps in any recommended CHD testing during the study period. Multivariate logistic regression examined the association of ADI on primary outcome after adjusting for age, sex, race, ethnicity, rurality, language, insurance, CHD anatomic type, and comorbidities.
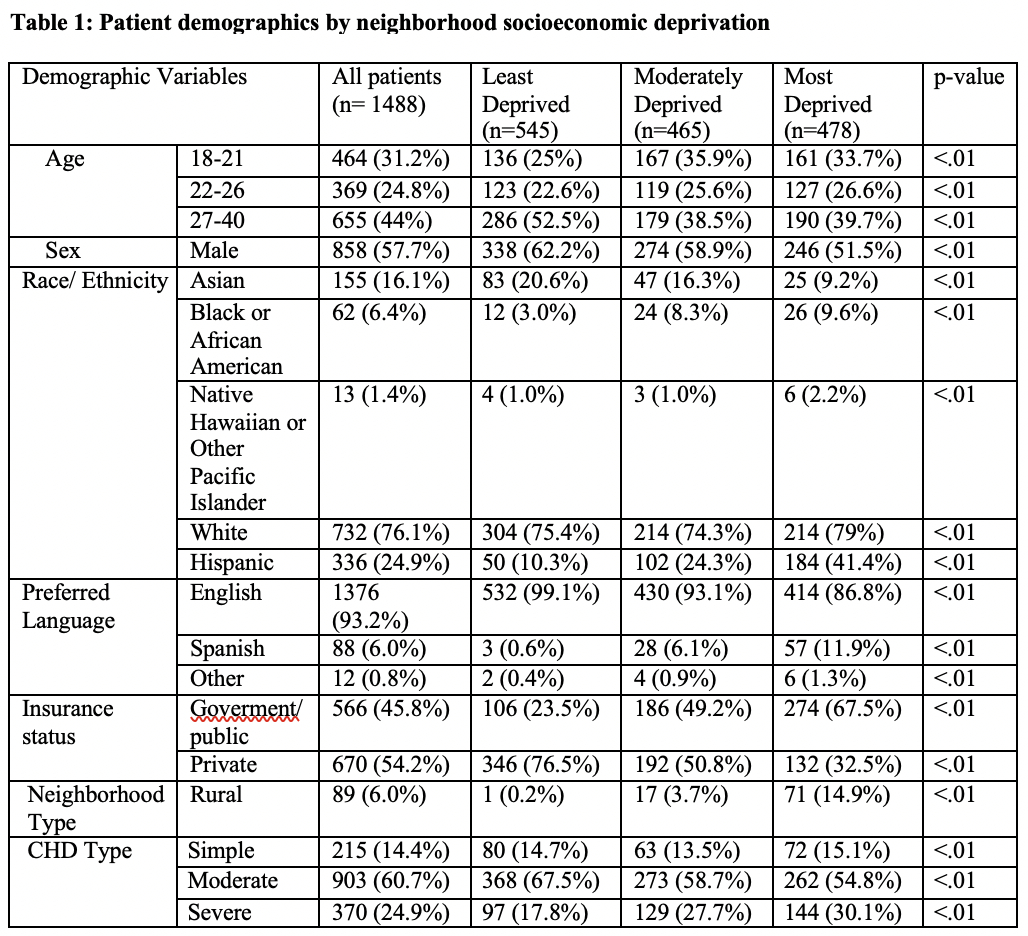
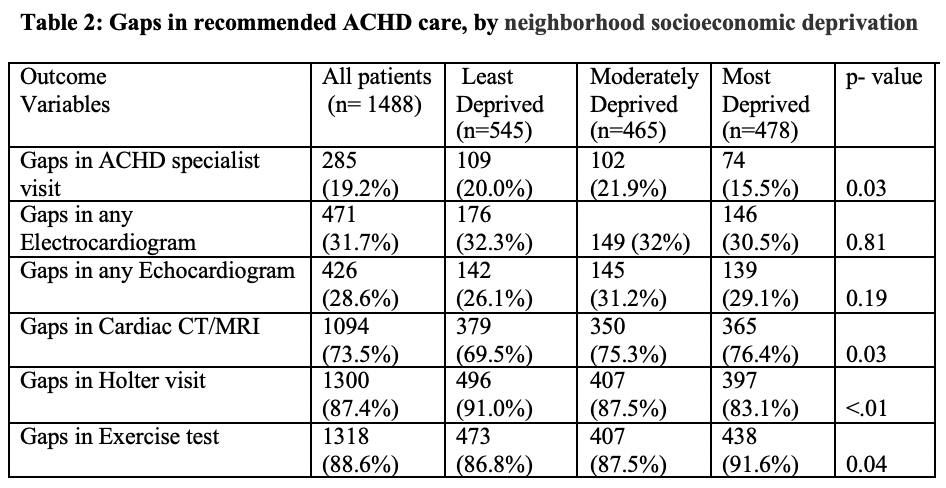
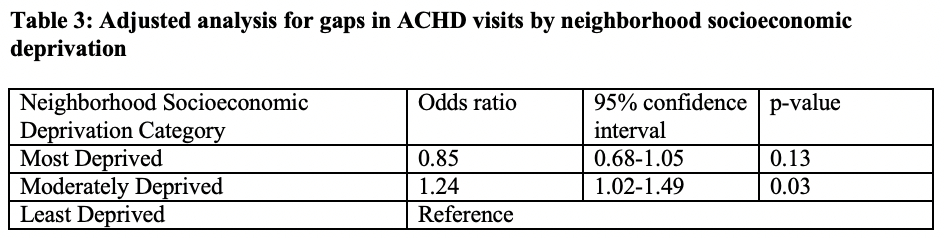
Results: Of 1,488 patients, 31% were moderately deprived, 32% were most deprived. Moderately and most deprived patients were more likely to be younger, female, non-Asian, Hispanic, Spanish speaking, on government insurance, rural, and have severe CHD and physiological class B-D medical conditions (Table 1). Moderately deprived patients were significantly more likely to have gaps in ACHD specialist visits as well as gaps in electrocardiogram, echocardiogram, and Holter tests compared to the most deprived group (Table 2). On adjusted analysis, moderately deprived patients were 1.24 times more likely to have gaps in ACHD visits compared to those least deprived (Table 3).
Conclusion: Patients with moderate socioeconomic deprivation experience more gaps in ACHD visits and certain recommended CHD testing. These findings underscore the need for interventions aimed at patients who may typically receive less formal social and governmental support and have fewer interactions with the health system.
Objective: To evaluate the effect of neighborhood socioeconomic deprivation on gaps in adult CHD specialist visits for young adults with CHD
Methods: We conducted a retrospective observational study using electronic health record data from University of California, San Francisco. Our inclusion criteria were patients aged 18-40 who had at least one encounter between 2018 and 2022. The independent variable was neighborhood socioeconomic deprivation measured by the area deprivation index (ADI), a composite index of census-derived indicators. Patients with ADI score of 1-2 were considered least deprived, those with 3-5 as moderately deprived, and those 7-10 as most deprived. The primary outcome was gaps in any ACHD specialist visit during the study period. Secondary outcome was gaps in any recommended CHD testing during the study period. Multivariate logistic regression examined the association of ADI on primary outcome after adjusting for age, sex, race, ethnicity, rurality, language, insurance, CHD anatomic type, and comorbidities.
Results: Of 1,488 patients, 31% were moderately deprived, 32% were most deprived. Moderately and most deprived patients were more likely to be younger, female, non-Asian, Hispanic, Spanish speaking, on government insurance, rural, and have severe CHD and physiological class B-D medical conditions (Table 1). Moderately deprived patients were significantly more likely to have gaps in ACHD specialist visits as well as gaps in electrocardiogram, echocardiogram, and Holter tests compared to the most deprived group (Table 2). On adjusted analysis, moderately deprived patients were 1.24 times more likely to have gaps in ACHD visits compared to those least deprived (Table 3).
Conclusion: Patients with moderate socioeconomic deprivation experience more gaps in ACHD visits and certain recommended CHD testing. These findings underscore the need for interventions aimed at patients who may typically receive less formal social and governmental support and have fewer interactions with the health system.
More abstracts on this topic:
3-Minute Heart Health App: A Feasibility Study
Abdulkarim Iya, Metzger Joseph, Stovitz Steven, Van't Hof Jeremy
A Comparative Analysis of Social Demographic and Clinical Factors for Screening for Peripheral Artery Disease in Adult Patients from Primary Care ClinicsLane Rashon, Jackson Pasha, Anokwuru Ferdinand, Dillard Naomi, Nerlekar Ridhima