Final ID: MP2641
Cavo-Tricuspid Isthmus Ablation in Atrial Flutter with Uncorrected Ebstein’s Anomaly: A Scoping Review
Abstract Body (Do not enter title and authors here): Background: Ebstein’s anomaly (EA) is a rare congenital heart defect characterized by apical displacement and abnormal development of the tricuspid valve, resulting in right atrial enlargement and a predisposition to atrial arrhythmias. Typical atrial flutter (AFL), frequently involving the cavo-tricuspid isthmus (CTI), affects up to 21% of individuals with EA. While CTI ablation is the standard of care for typical AFL, it is technically challenging in EA due to complex and distorted right heart anatomy.
Objective: To evaluate the current literature on the procedural success, safety, and long-term outcomes of CTI ablation in patients with uncorrected Ebstein’s anomaly.
Methods: A scoping review was conducted per PRISMA-ScR guidelines. We systematically searched PubMed, EMBASE, and Scopus using terms such as “Ebstein anomaly,” “atrial flutter,” and “cavo-tricuspid isthmus ablation.” Studies reporting on CTI ablation in patients with uncorrected EA were included. Data on procedural characteristics, success rates, complications, arrhythmia recurrence, and use of adjunctive ablation were extracted and synthesized.
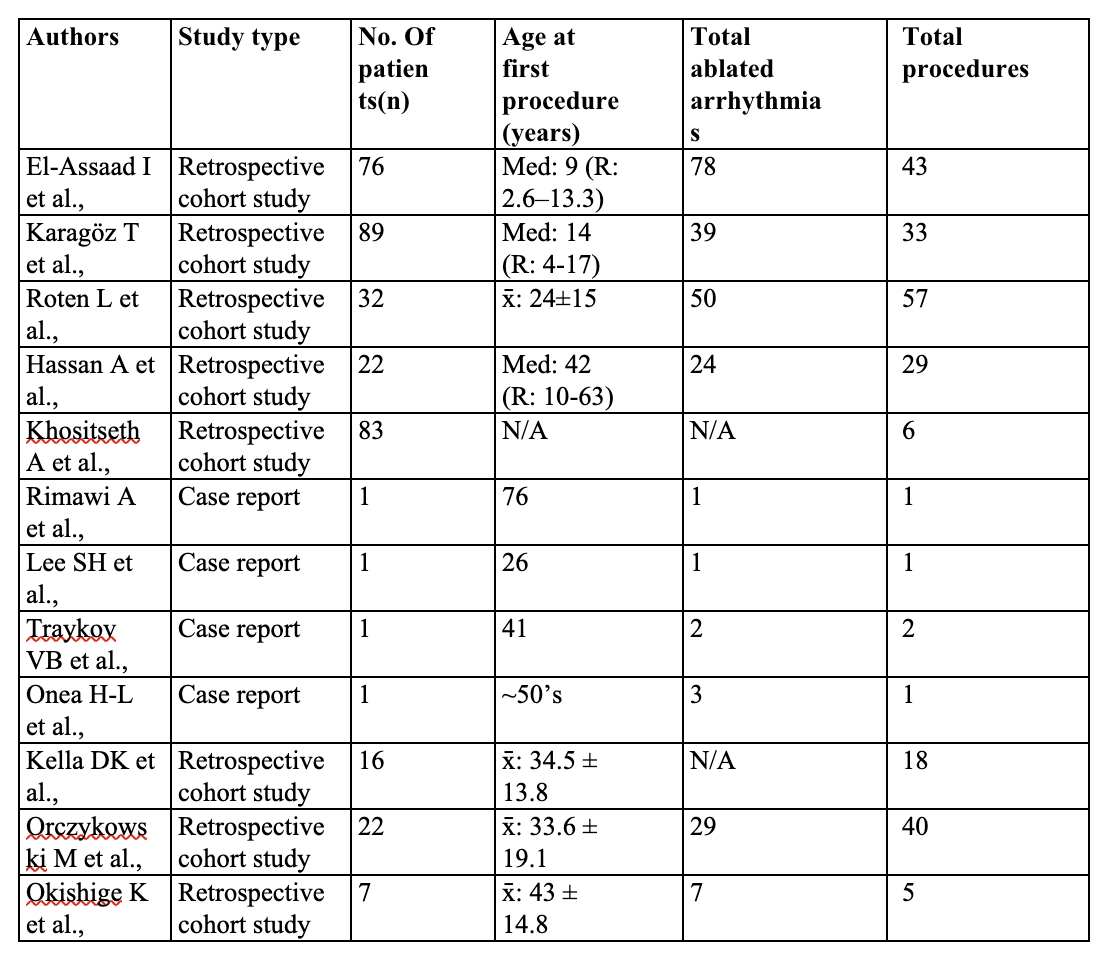
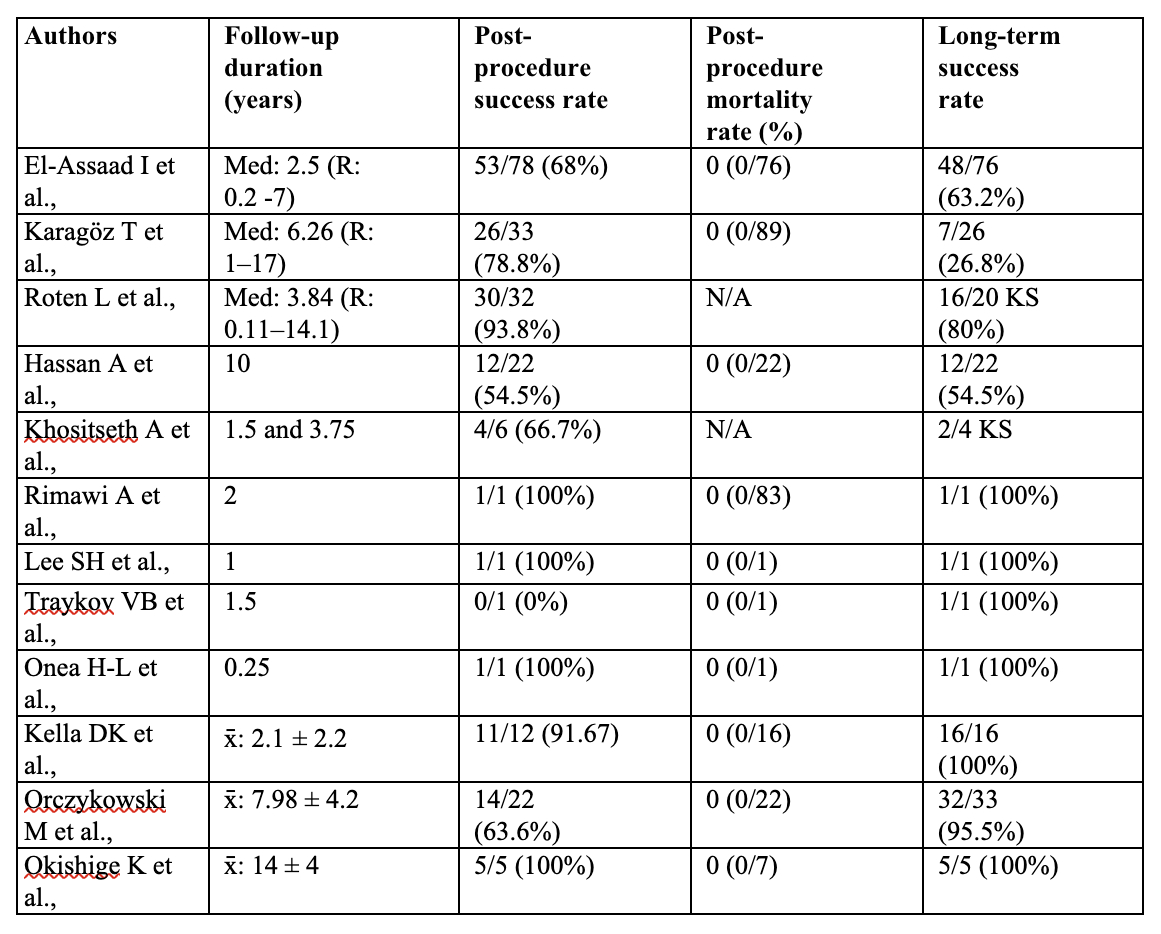
Results: Twelve studies encompassing 351 patients with EA undergoing radiofrequency catheter ablation for atrial arrhythmias were included. A total of 234 arrhythmias were targeted across 263 ablation procedures. Immediate post-procedural success—defined as arrhythmia termination following the first ablation—was reported in 158 of 214 patients (73.8%). Long-term success—defined as sustained arrhythmia-free survival after all ablation procedures—was achieved in 142 of 206 patients (63.9%). Detailed outcomes per study are summarized in Tables 1 & 2.
Conclusion: CTI ablation in uncorrected EA is both feasible and effective, despite anatomical challenges such as tricuspid valve displacement, right atrial enlargement, and atrialized right ventricular tissue. Acute success rates are high (73–94%), and recurrence of typical AFL is relatively low (~6.3%). However, long-term follow-up reveals a high incidence (25–50%) of new-onset atrial fibrillation. Intracardiac echocardiography enhances procedural precision and safety. While adjunctive pulmonary vein isolation (PVI) may help mitigate AF development, it is not routinely performed. Individualized ablation strategies informed by detailed anatomical assessment are critical to optimizing patient outcomes in this complex population.
Objective: To evaluate the current literature on the procedural success, safety, and long-term outcomes of CTI ablation in patients with uncorrected Ebstein’s anomaly.
Methods: A scoping review was conducted per PRISMA-ScR guidelines. We systematically searched PubMed, EMBASE, and Scopus using terms such as “Ebstein anomaly,” “atrial flutter,” and “cavo-tricuspid isthmus ablation.” Studies reporting on CTI ablation in patients with uncorrected EA were included. Data on procedural characteristics, success rates, complications, arrhythmia recurrence, and use of adjunctive ablation were extracted and synthesized.
Results: Twelve studies encompassing 351 patients with EA undergoing radiofrequency catheter ablation for atrial arrhythmias were included. A total of 234 arrhythmias were targeted across 263 ablation procedures. Immediate post-procedural success—defined as arrhythmia termination following the first ablation—was reported in 158 of 214 patients (73.8%). Long-term success—defined as sustained arrhythmia-free survival after all ablation procedures—was achieved in 142 of 206 patients (63.9%). Detailed outcomes per study are summarized in Tables 1 & 2.
Conclusion: CTI ablation in uncorrected EA is both feasible and effective, despite anatomical challenges such as tricuspid valve displacement, right atrial enlargement, and atrialized right ventricular tissue. Acute success rates are high (73–94%), and recurrence of typical AFL is relatively low (~6.3%). However, long-term follow-up reveals a high incidence (25–50%) of new-onset atrial fibrillation. Intracardiac echocardiography enhances procedural precision and safety. While adjunctive pulmonary vein isolation (PVI) may help mitigate AF development, it is not routinely performed. Individualized ablation strategies informed by detailed anatomical assessment are critical to optimizing patient outcomes in this complex population.
More abstracts on this topic:
Catheter Ablation for Atrial Fibrillation May Improve Mortality in Patients with Heart Failure with Preserved Ejection Fraction, Similar to Reduced Ejection Fraction
Benjamin Patrick, Oyenubi Olamide, Fohle Emmanuel, Shahmoradi Vahe, Khan Dawlat, Maryniak Andrii
A CRISPR-Activation CROP-seq Screen Identifies HMGN1 as a Dosage-Sensitive Regulator of Heart Defects in Down SyndromeRanade Sanjeev, Mital Rahul, Boileau Ryan, Koback Frances, Padmanabhan Arun, Merriman Alexander, Wallace Langley, Nguyen Annie, Poulis Nikolaus, Gifford Casey, Pollard Katherine, Li Feiya, Srivastava Deepak, Whalen Sean, Angelo Pelonero, Ye Lin, Huang Yu, Brand Abigail, Nishino Tomohiro, Costa Mauro