Final ID: MP1379
Co-existence And Prognosis of 18FDG-avidity And Genetic Cardiomyopathies
Objectives: To evaluate the prevalence of pathogenic and likely pathogenic (P/LP) variants in 18FDG-avid cardiomyopathy and assess the association between FDG-avidity, genetic variants, and heart failure outcomes.
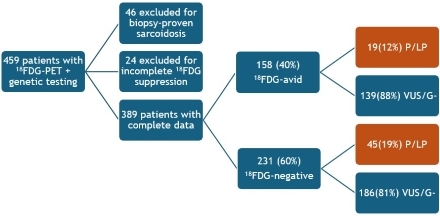
Methods: A multi-center retrospective cohort study combined patients from three centers who underwent both a cardiac 18FDG-PET scan and commercial genetic testing for genetic cardiomyopathies. We excluded patients with biopsy-proven sarcoidosis, as well as those with incomplete 18FDG suppression. Chi-square tests were used to compare between group characteristics, and Kaplan-Meier survival analyses were performed to evaluate time to event outcomes, including a composite of death, LVAD implantation, or heart transplant, based on 18FDG-avidity and genetic status.
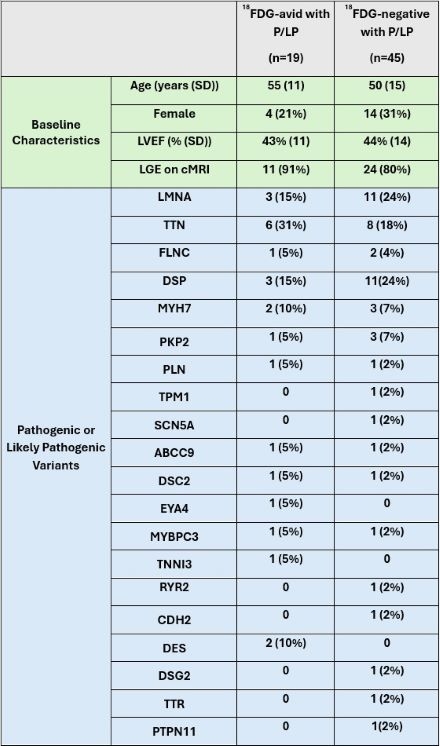
Results: Among 459 patients who underwent both a cardiac 18FDG-PET scan and genetic testing, 389 (33% female; mean age 54 years) met the inclusion criteria. 18FDG-avidity was identified in 158 (40%). Within this subgroup, 19 (12%) had a P/LP variant compared with 19% of the 18FDG-negative patients (p=0.051; Figure 1). Baseline characteristics were similar, and a wide array of genes was implicated in 18FDG-avid cardiomyopathy (Figure 2).
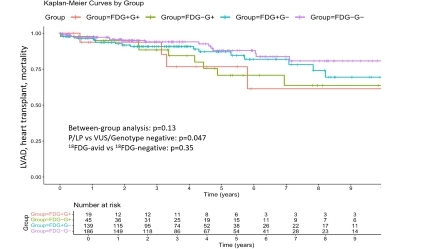
Survival analysis revealed no significant difference between the four genotype-FDG subgroups (p=0.13, Figure 3), and 18FDG-avidity was not significantly associated with the composite endpoint in the overall cohort (p=0.35), nor within the subset of patients with P/LP variants (p=0.84), suggesting that 18FDG-avidity did not predict clinical outcomes. The presence of a P/LP variant was associated with an increased incidence of the composite endpoint (p=0.047).
Conclusion: 18FDG-avidity is frequently noted in patients with genetic cardiomyopathy, but was not associated with adverse clinical outcomes, suggesting it may not reflect clinically relevant inflammation. P/LP variants were significantly associated with survival outcomes, highlighting the value of genetic testing in patients with suspected inflammatory cardiomyopathy.
- Tabaghi, Shiva ( University of Washington , Seattle , Washington , United States )
- Di Carli, Marcelo ( Brigham and Women's Hospital , Boston , Massachusetts , United States )
- Chatterjee, Neal ( University of Washington , Seattle , Washington , United States )
- Cheng, Richard ( University of Washington , Seattle , Washington , United States )
- Stempien-otero, April ( University of Washington , Seattle , Washington , United States )
- Levin, Benjamin ( Oregon Health & Science University , Portland , Oregon , United States )
- Divakaran, Sanjay ( Brigham and Women's Hospital , Boston , Massachusetts , United States )
- Nazer, Babak ( University of Washington , Seattle , Washington , United States )
- Bevan, Graham ( University of Washington , Seattle , Washington , United States )
- Hankinson, Stephen ( Brigham and Women's Hospital , Boston , Massachusetts , United States )
- Lal, Mallika ( Oregon Health & Science University , Portland , Oregon , United States )
- Pico, Madison ( Oregon Health & Science University , Portland , Oregon , United States )
- Lakdawala, Neal ( Brigham and Women's Hospital , Boston , Massachusetts , United States )
- Sauer, William ( Brigham and Women's Hospital , Boston , Massachusetts , United States )
- Tedrow, Usha ( Brigham and Women's Hospital , Boston , Massachusetts , United States )
- Blankstein, Ron ( Brigham and Women's Hospital , Boston , Massachusetts , United States )
Meeting Info:
Session Info:
Sunday, 11/09/2025 , 03:15PM - 04:25PM
Moderated Digital Poster Session
More abstracts on this topic:
Oliver Shannon, Ward Cameron
A new genetic model organism for primate-specific cardiac function and diseaseChang Stephen, Albertelli Megan, Quertermous Thomas, Wright Patricia, Terrien Jeremy, Aujard Fabienne, Wu Joseph, Krasnow Mark, Karanewsky Caitlin, Pendleton Jozeph, Ren Lu, Anzeraey Aude, Froelicher Victor, Liang David, Razafindrakoto Andriamahery, Ravelonjanahary Noeline
More abstracts from these authors:
Zia Abdul, Lal Mallika, Nazer Babak, Levin Benjamin, Masri Ahmad
Prevalence of FDG-avidity in genetic cardiomyopathy and prediction of arrhythmic free survivalBevan Graham, Nazer Babak, Tabaghi Shiva, Lal Mallika, Memar Kimia, Pico Madison, Cheng Richard, Stempien-otero April, Chatterjee Neal, Levin Benjamin