Final ID: MP1693
National Outcomes of Concomitant Left Atrial Appendage Management and TAVR in Patients with Atrial Fibrillation
Abstract Body (Do not enter title and authors here): Introduction:
Guideline recommendations for patients with atrial fibrillation undergoing cardiac surgery have considered atrial appendage management for the past decade. Recently, the WATCH-TAVR trial compared the safety of concomitant left atrial appendage occlusion (LAAO) for patients with atrial fibrillation undergoing TAVR and found that TAVR+LAAO was non-inferior to medical management. We sought to compare the rates of left atrial appendage management in patients undergoing TAVR vs. SAVR and then further examine the outcomes of TAVR + LAAO versus TAVR alone.
Hypothesis:
What is the rate of LAA management in TAVR paitents with atrial fibrillation compared to SAVR patients and is there a difference in a composite of death, stroke or bleeding in patients for patients with TAVR undergoing LAAO within 1 month of their TAVR procedure?
Methods:
Administrative billing data from the Centers for Medicare and Medicaid Services were used to identify patients from 2012 through 2020 with atrial fibrillation or atrial flutter undergoing either SAVR or TAVR. Comorbidities and left atrial appendage management, either operative or endovascular were identified for further patient stratification comparing patients undergoing TAVR with LAAO within 1 month versus those undergoing TAVR alone. Univariate and Kaplan-Meier time-to-event analyses were conducted to compare the primary outcome of a composite of death, stroke or major bleeding and their individual components.
Results:
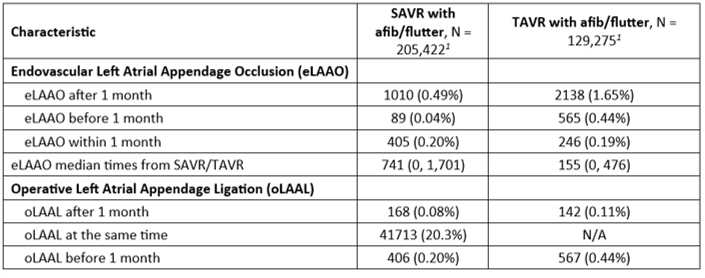
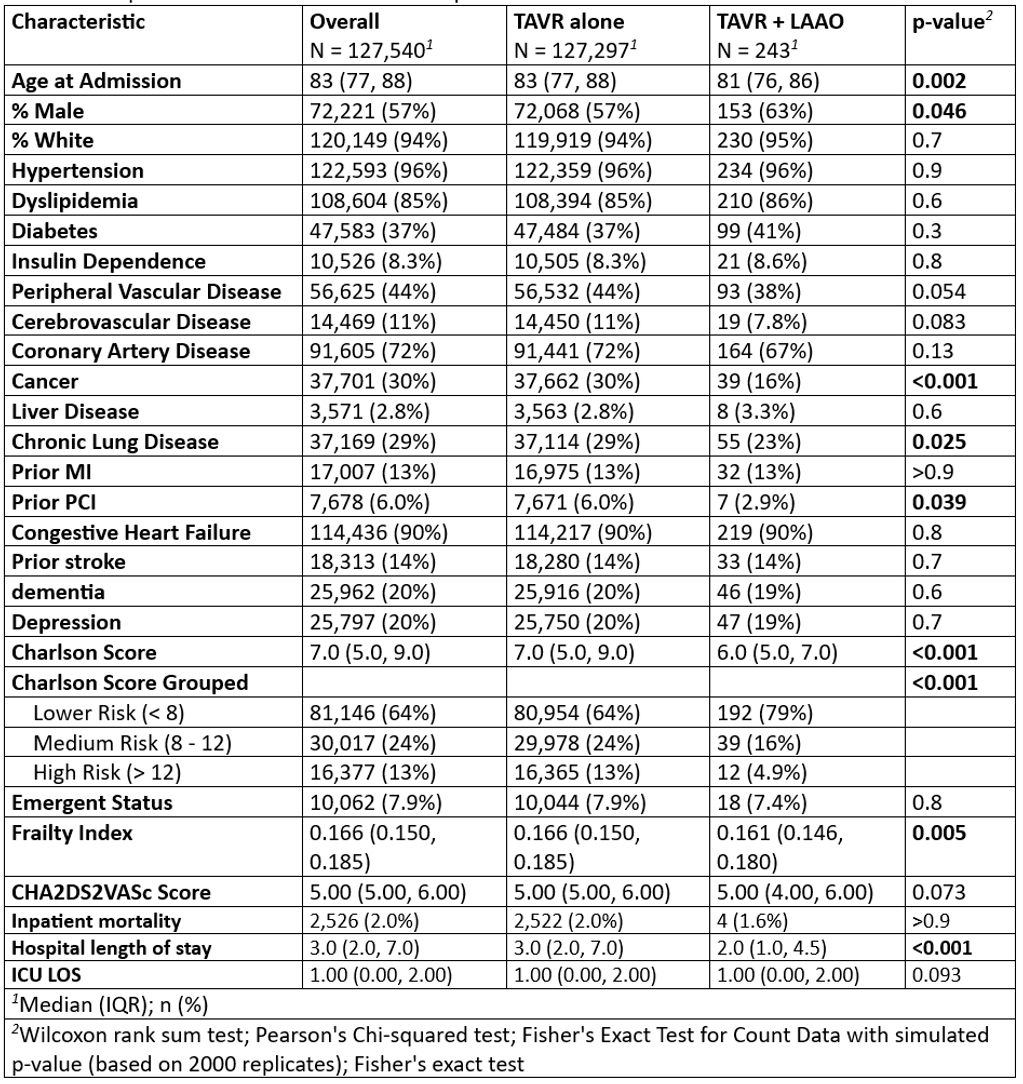
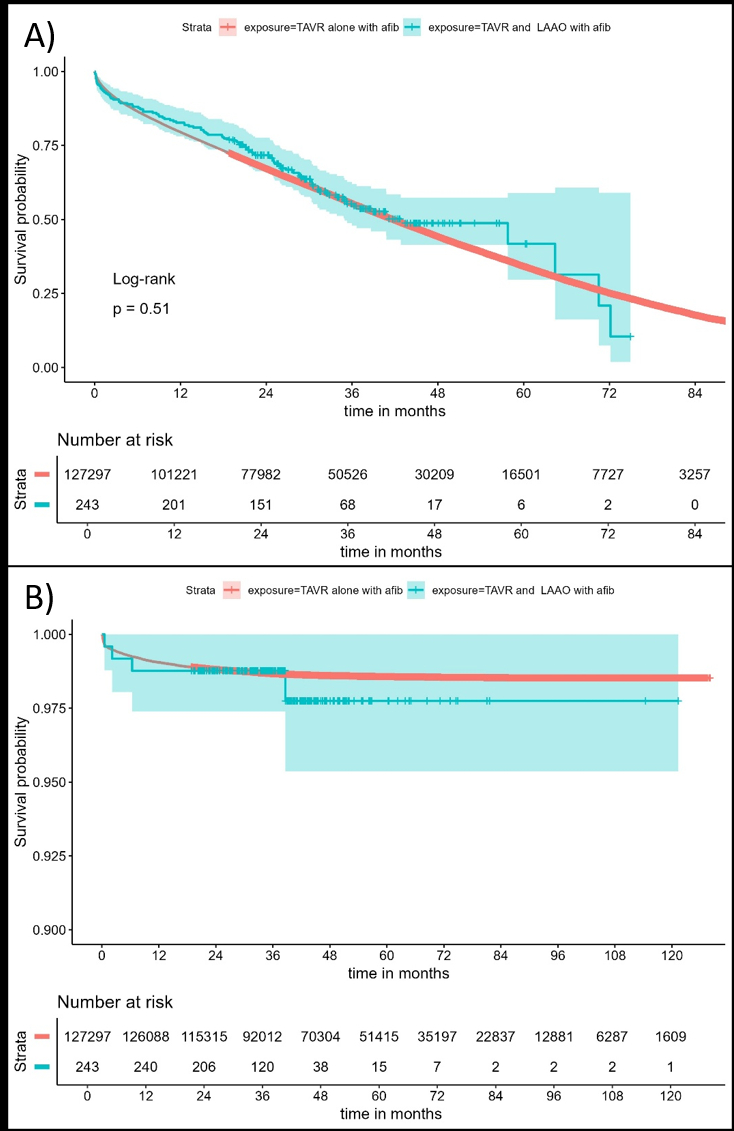
205,422 SAVR patients and 129,275 TAVR patients were identified. 20.3% of the SAVR patients underwent LAAL at the time of their surgery versus 0.19% (246/129,275) of TAVR patients (Table 1). Of the TAVR patients with afib/aflutter, 0.88% had previously been treated with either operative or endovascular LAAO and were excluded. TAVR+LAAO patients were slightly younger at time of procedure, with lower Charlson Comorbidity and Frailty indexes but a similar median CHA2DS2VASc score of 5. There was no difference in hospital mortality between the two groups, although TAVR+LAAO had slightly lower hospital length of stay. There was no difference in primary outcome between TAVR vs. TAVR+LAAO (Figure 1A) nor was there any difference in readmission for stroke (Figure 1B).
Conclusions:
Our data shows that LAAO within 1 month of TAVR can be done safely but does not lead to differences in stroke or a composite of mortality, stroke or bleeding in these patients.
Guideline recommendations for patients with atrial fibrillation undergoing cardiac surgery have considered atrial appendage management for the past decade. Recently, the WATCH-TAVR trial compared the safety of concomitant left atrial appendage occlusion (LAAO) for patients with atrial fibrillation undergoing TAVR and found that TAVR+LAAO was non-inferior to medical management. We sought to compare the rates of left atrial appendage management in patients undergoing TAVR vs. SAVR and then further examine the outcomes of TAVR + LAAO versus TAVR alone.
Hypothesis:
What is the rate of LAA management in TAVR paitents with atrial fibrillation compared to SAVR patients and is there a difference in a composite of death, stroke or bleeding in patients for patients with TAVR undergoing LAAO within 1 month of their TAVR procedure?
Methods:
Administrative billing data from the Centers for Medicare and Medicaid Services were used to identify patients from 2012 through 2020 with atrial fibrillation or atrial flutter undergoing either SAVR or TAVR. Comorbidities and left atrial appendage management, either operative or endovascular were identified for further patient stratification comparing patients undergoing TAVR with LAAO within 1 month versus those undergoing TAVR alone. Univariate and Kaplan-Meier time-to-event analyses were conducted to compare the primary outcome of a composite of death, stroke or major bleeding and their individual components.
Results:
205,422 SAVR patients and 129,275 TAVR patients were identified. 20.3% of the SAVR patients underwent LAAL at the time of their surgery versus 0.19% (246/129,275) of TAVR patients (Table 1). Of the TAVR patients with afib/aflutter, 0.88% had previously been treated with either operative or endovascular LAAO and were excluded. TAVR+LAAO patients were slightly younger at time of procedure, with lower Charlson Comorbidity and Frailty indexes but a similar median CHA2DS2VASc score of 5. There was no difference in hospital mortality between the two groups, although TAVR+LAAO had slightly lower hospital length of stay. There was no difference in primary outcome between TAVR vs. TAVR+LAAO (Figure 1A) nor was there any difference in readmission for stroke (Figure 1B).
Conclusions:
Our data shows that LAAO within 1 month of TAVR can be done safely but does not lead to differences in stroke or a composite of mortality, stroke or bleeding in these patients.
More abstracts on this topic:
A Delayed Diagnosis of Anti-HMG-CoA Reductase Immune-Mediated Necrotizing Myopathy
Jadhav Reshma, Shekar Arush, Westenhaver Zack, Skandhan Amith
A Fat Chance: Paradoxical Embolic Stroke from Lipomatous Hypertrophy of the Interatrial SeptumKalathoor Abraham