Final ID: MP1445
Association of Body Size and Shape Metrics with Atherosclerotic Cardiovascular Disease and Mortality: Ethnic Differences in a Nationally Representative Cohort of U.S. Adults
Abstract Body (Do not enter title and authors here): Background
BMI is widely used to assess adiposity and cardiometabolic risk, yet its utility varies by race/ethnicity. Alternative indices such as Body Roundness Index (BRI) and A Body Shape Index (ABSI) may offer improved risk stratification, but their utility remains unclear in the ethnically diverse U.S. population.
Research Question
We evaluated associations of BMI, BRI, and ABSI with prevalent ASCVD and all-cause mortality, and determine whether these associations vary by race/ethnicity.
Methods
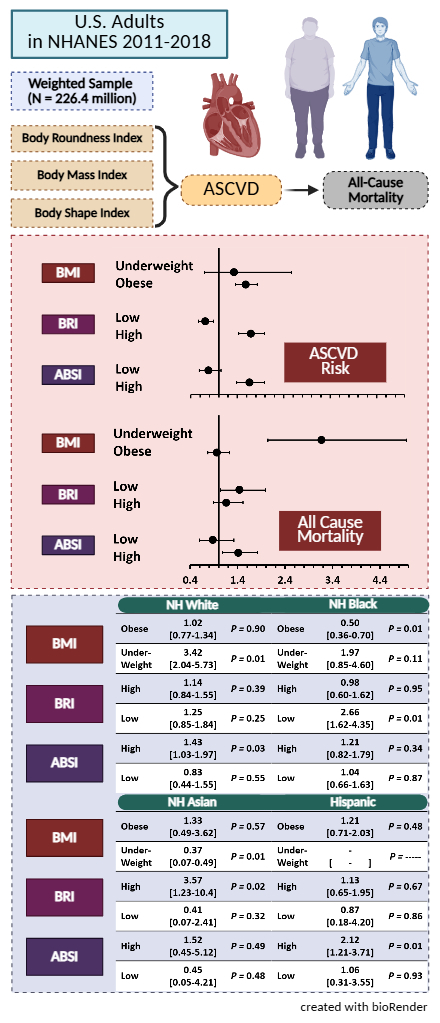
Adults from the National Health and Nutrition Examination Survey cycles 2011-2018 (N = 21,294; weighted 226.4 million) were analyzed. BMI was categorized per WHO cutoffs (obesity ≥30 kg/m2, underweight <18.5 kg/m2, ≥27.5 kg/m2 for obese Asian adults). BRI and ABSI were divided into quartiles, and the interquartile range was set as reference. Survey weighted regression models were employed to estimate the odds of prevalent ASCVD and the hazards of mortality. Subgroup analyses tested for racial/ethnic differences.
Results
Obesity as defined by BMI, BRI, and ABSI were all associated with higher odds of ASCVD (aOR 1.58 [1.36-1.83]; 1.69 [1.43-1.99]; 1.66 [1.39-1.98] respectively). Underweight BMI was associated with increased mortality risk (aHR 3.18 [2.04-4.95]), while obesity showed no significant association. However, a high ABSI 1.41 [1.08-1.82] and low BRI 1.44 [1.04-1.98] were associated with mortality in the overall population. Subgroup analyses revealed significant ethnic differences that persisted after comprehensive multivariable adjustment (Figure). Among White adults, underweight BMI and high ABSI predicted mortality. In Asian adults, high BRI conferred greatest risk, while underweight BMI was inversely associated with mortality. In Black adults, higher BMI was associated with lower mortality, and a low BRI was associated with higher risk. For Hispanic adults, high ABSI was the only significant mortality predictor.
Conclusion
Our findings suggest that BMI, BRI, and ABSI have differential predictive value for mortality across racial/ethnic groups. While BMI alone may underestimate risk, BRI and ABSI offer nuanced risk stratification, particularly in non-White populations. These results underscore the need for racial/ethnic conscious anthropometric risk assessments in clinical and public health settings.
BMI is widely used to assess adiposity and cardiometabolic risk, yet its utility varies by race/ethnicity. Alternative indices such as Body Roundness Index (BRI) and A Body Shape Index (ABSI) may offer improved risk stratification, but their utility remains unclear in the ethnically diverse U.S. population.
Research Question
We evaluated associations of BMI, BRI, and ABSI with prevalent ASCVD and all-cause mortality, and determine whether these associations vary by race/ethnicity.
Methods
Adults from the National Health and Nutrition Examination Survey cycles 2011-2018 (N = 21,294; weighted 226.4 million) were analyzed. BMI was categorized per WHO cutoffs (obesity ≥30 kg/m2, underweight <18.5 kg/m2, ≥27.5 kg/m2 for obese Asian adults). BRI and ABSI were divided into quartiles, and the interquartile range was set as reference. Survey weighted regression models were employed to estimate the odds of prevalent ASCVD and the hazards of mortality. Subgroup analyses tested for racial/ethnic differences.
Results
Obesity as defined by BMI, BRI, and ABSI were all associated with higher odds of ASCVD (aOR 1.58 [1.36-1.83]; 1.69 [1.43-1.99]; 1.66 [1.39-1.98] respectively). Underweight BMI was associated with increased mortality risk (aHR 3.18 [2.04-4.95]), while obesity showed no significant association. However, a high ABSI 1.41 [1.08-1.82] and low BRI 1.44 [1.04-1.98] were associated with mortality in the overall population. Subgroup analyses revealed significant ethnic differences that persisted after comprehensive multivariable adjustment (Figure). Among White adults, underweight BMI and high ABSI predicted mortality. In Asian adults, high BRI conferred greatest risk, while underweight BMI was inversely associated with mortality. In Black adults, higher BMI was associated with lower mortality, and a low BRI was associated with higher risk. For Hispanic adults, high ABSI was the only significant mortality predictor.
Conclusion
Our findings suggest that BMI, BRI, and ABSI have differential predictive value for mortality across racial/ethnic groups. While BMI alone may underestimate risk, BRI and ABSI offer nuanced risk stratification, particularly in non-White populations. These results underscore the need for racial/ethnic conscious anthropometric risk assessments in clinical and public health settings.
More abstracts on this topic:
Assessment performance of the AHA PREVENT equations in disaggregated Asian and Hispanic Subgroups
Yan Xiaowei, Bacong Adrian, Huang Qiwen, Husby Hannah, Jose Powell, Palaniappan Latha, Rodriguez Fatima
Black and Hispanic Patients Have Lower Survival Outcomes Than White Patients in Out-of-Hospital Cardiac Arrests Witnessed by 9-1-1 RespondersPande Madhura, Ornato Joseph, Powell Stephen, Starks Monique, Yow Eric, Chan Paul, Blewer Audrey, Mark Daniel, Al-khalidi Hussein, Sasson Comilla, Mcnally Bryan, Al-araji Rabab