Final ID: MP1839
Fatty Degeneration of Nonhemorrhagic Myocardial Infarction: a Longitudinal PET/MRI Study with Histological Validation
Abstract Body (Do not enter title and authors here): Background: Fatty degeneration of infarcted myocardium, also known as lipomatous metaplasia (LM), is a highly prevalent phenomenon linked with high incidence of major adverse cardiovascular events. Notably, the transformation of dense post-myocardial infarction (MI) scar into a compressible and mobile adipose tissue impairs local contraction and electrical conductivity. So far, LM has been reported in both humans and animal models (canine, ovine, rabbit, mouse). In recent study using a canine model, LM was observed in hemorrhagic (HEMO+) but not in nonhemorrhagic (HEMO-) MIs. Residual iron deposits in the HEMO+ MI have been shown to promote prolonged inflammation culminating in LM. However, it remains unknown whether the absence of LM in HEMO- MI is observable across species, and whether HEMO- and HEMO+ MIs indeed exhibit different metabolic phenotypes.
Methods: Ten pigs underwent a 90-minute ischemia-reperfusion in the left anterior descending artery, followed by T2*, LGE, cine, and 18FDG-PET/MRI at Day 5 and Week 12 post-MI. At Day 5, HEMO+ MIs were identified by T2* as hypointense core (≥1 mL) within the MI zone. Remote myocardium FDG uptake was suppressed by 48-hour ketogenic diet, 12-hour fasting, and 2000 U heparin injection 15 minutes before FDG administration. LGE and PET images were fused to compute target-to-background ratio (TBR). At Week 12, hearts were explanted for histological analysis using Masson’s trichrome and Prussian Blue stains.
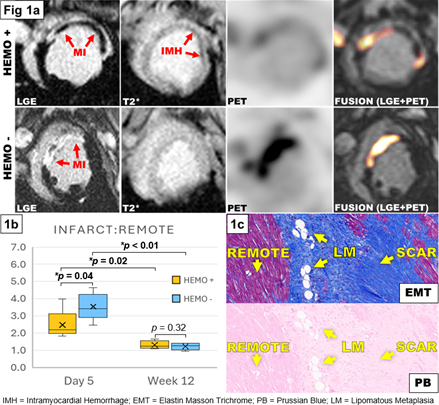
Results: Comparing HEMO+ (n=5) and HEMO- (n=5) groups at Day 5 (Fig 1a), there was: (i) increased infarct size in HEMO+ (HEMO+=25.8±3.5%LV; HEMO-=17.5±3.7%LV; p<0.01); (ii) decreased ejection fraction (EF) in HEMO+ (HEMO+=32.1±3.4%; HEMO-=42.9±7.0%; p=0.01); (iii) decreased infarct:remote TBR in HEMO+ (p=0.04)(Fig 1b). At Week 12, there was: (i) no difference in infarct size (HEMO+=9.6±2.0%LV; HEMO-=7.6±2.7%LV; p=0.12); (ii) reduced EF in HEMO+ (HEMO+=35.6±6.7%; HEMO-=43.4±3.9%; p=0.03); (iii) no difference in infarct:remote TBR (p=0.32)(Fig 1b). Histological analysis revealed individual adipose cells in MI scar in both HEMO+ and iron-deposit-negative HEMO- groups (Fig 1c).
Conclusions: By comparing MIs of same chronicity, we provide evidence that LM occurs in both HEMO+ and HEMO- MIs. Furthermore, we demonstrate for the first time that reperfused MIs undergoing LM, regardless of infarct size and hemorrhage, exhibit similar metabolic phenotype, suggesting that LM may be independent from iron-related inflammation.
Methods: Ten pigs underwent a 90-minute ischemia-reperfusion in the left anterior descending artery, followed by T2*, LGE, cine, and 18FDG-PET/MRI at Day 5 and Week 12 post-MI. At Day 5, HEMO+ MIs were identified by T2* as hypointense core (≥1 mL) within the MI zone. Remote myocardium FDG uptake was suppressed by 48-hour ketogenic diet, 12-hour fasting, and 2000 U heparin injection 15 minutes before FDG administration. LGE and PET images were fused to compute target-to-background ratio (TBR). At Week 12, hearts were explanted for histological analysis using Masson’s trichrome and Prussian Blue stains.
Results: Comparing HEMO+ (n=5) and HEMO- (n=5) groups at Day 5 (Fig 1a), there was: (i) increased infarct size in HEMO+ (HEMO+=25.8±3.5%LV; HEMO-=17.5±3.7%LV; p<0.01); (ii) decreased ejection fraction (EF) in HEMO+ (HEMO+=32.1±3.4%; HEMO-=42.9±7.0%; p=0.01); (iii) decreased infarct:remote TBR in HEMO+ (p=0.04)(Fig 1b). At Week 12, there was: (i) no difference in infarct size (HEMO+=9.6±2.0%LV; HEMO-=7.6±2.7%LV; p=0.12); (ii) reduced EF in HEMO+ (HEMO+=35.6±6.7%; HEMO-=43.4±3.9%; p=0.03); (iii) no difference in infarct:remote TBR (p=0.32)(Fig 1b). Histological analysis revealed individual adipose cells in MI scar in both HEMO+ and iron-deposit-negative HEMO- groups (Fig 1c).
Conclusions: By comparing MIs of same chronicity, we provide evidence that LM occurs in both HEMO+ and HEMO- MIs. Furthermore, we demonstrate for the first time that reperfused MIs undergoing LM, regardless of infarct size and hemorrhage, exhibit similar metabolic phenotype, suggesting that LM may be independent from iron-related inflammation.
More abstracts on this topic:
A Novel ECG Time-Frequency Eyeball Method for Robust Detection of Myocardial Infarction from Single-Channel ECG: A Preclinical Study
Alavi Rashid, Li Jiajun, Dai Wangde, Matthews Ray, Pahlevan Niema, Kloner Robert, Gharib Morteza
A Rare Cause of a Classic Presentation of NSTEMI: Case of 39-Year-Old Female with Hypothyroidism Induced MyocarditisQuadri Fayz, Qazi Mariam, Teague Taylor