Final ID: MP2438
Socioeconomic Predictors of Clinic Follow-Up in Adults with Congenital Heart Disease: A Logistic Regression Analysis
Abstract Body (Do not enter title and authors here): Background:
Adults with congenital heart disease (ACHD) are surviving longer due to medical advancements, but remain at risk for complications like heart failure and sudden cardiac death. Lifelong follow-up in specialized clinics is critical, though adherence is often low. Socioeconomic status (SES) is known to influence healthcare access; however, its impact on ACHD populations remains understudied. Understanding SES barriers to clinic attendance could inform strategies to enhance outcomes in this group.
Hypothesis:
We investigated whether SES indicators—smoking, alcohol use, drug use, marital status, employment, and insurance—predict clinic follow-up among ACHD patients. We hypothesized that socioeconomic factors would significantly influence adherence to follow-up.
Methods:
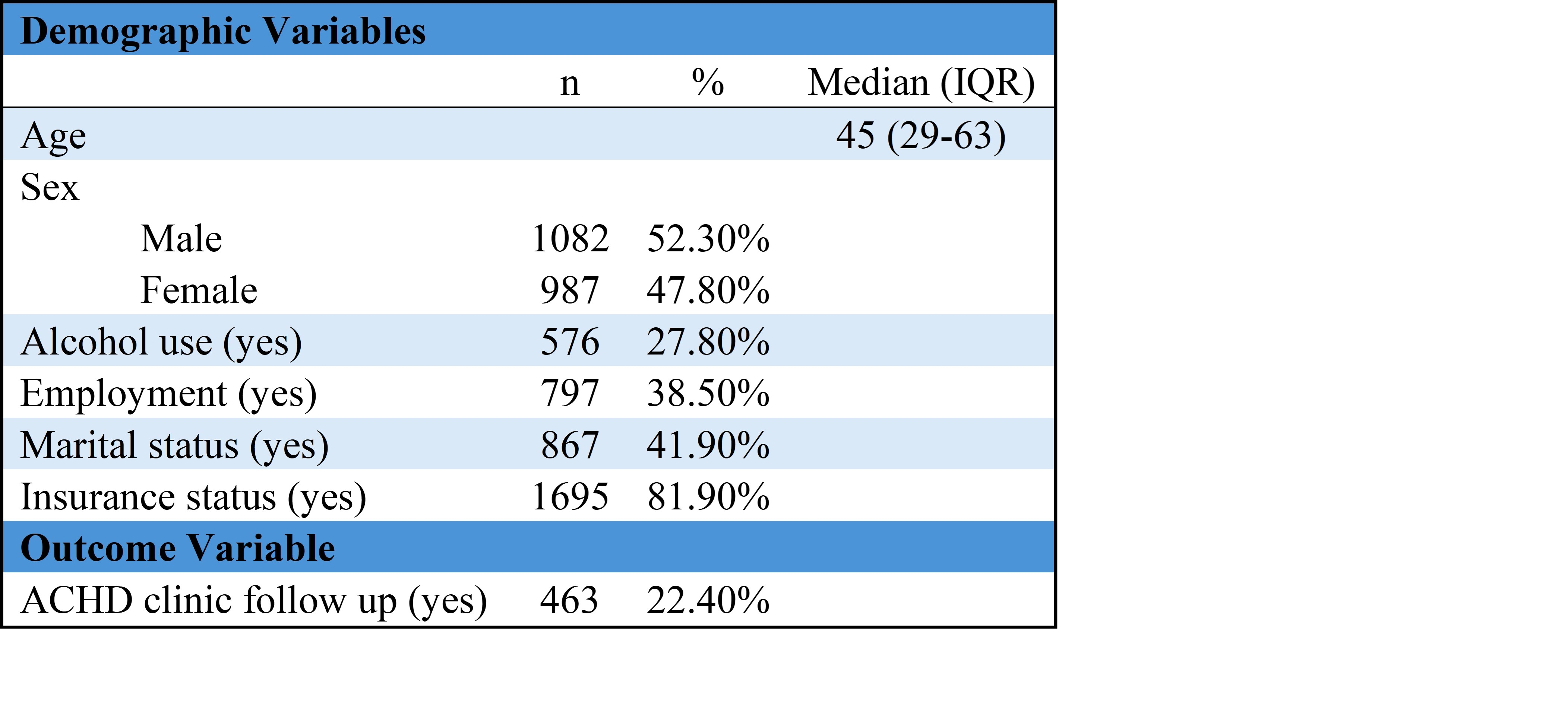
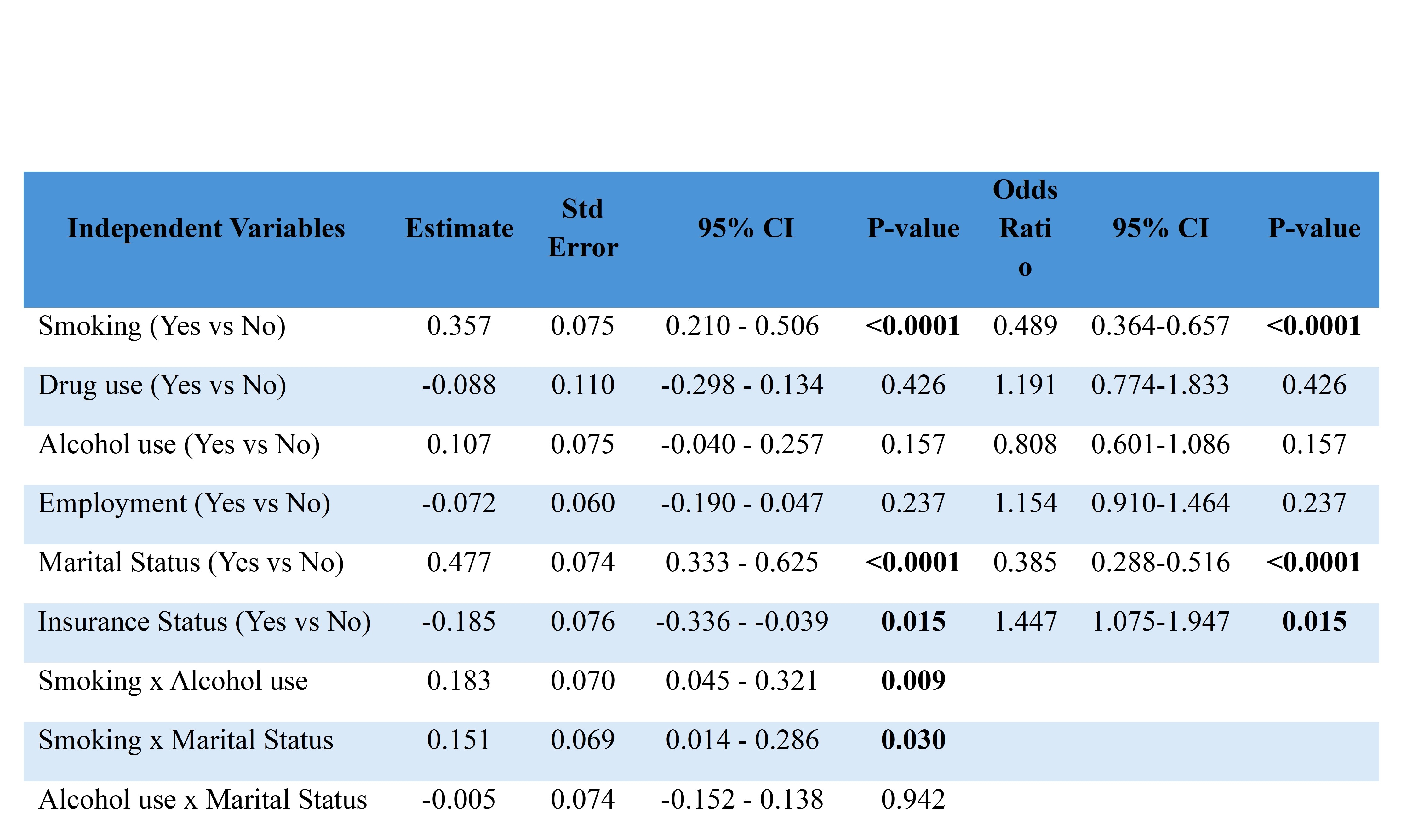
A retrospective analysis was conducted on 2,069 adults with ACHD using electronic health records from a single academic health system. The primary outcome was attendance at one follow-up visit at the ACHD clinic (Yes/No). Predictor variables were binarized for analysis. Logistic regression models were used to assess both unadjusted and adjusted associations, with interaction terms evaluated based on theoretical rationale. Model fit was assessed using AIC, lack-of-fit tests, and multicollinearity diagnostics.
Results:
Out of 2,069 patients, only 463 (22.4%) attended follow-up. In adjusted models, non-smokers had greater odds of follow-up (OR 0.49; 95% CI: 0.36–0.66; p < 0.0001). Patients without partners were more likely to follow up than those in relationships (OR 0.39; 95% CI: 0.29–0.52; p < 0.0001). Insurance coverage correlated positively with follow-up (OR 1.45; 95% CI: 1.08–1.95; p = 0.015). Drug use, alcohol use, and employment were not independently linked to follow-up, but significant interaction effects were found between smoking and alcohol use (p = 0.009) and smoking and marital status (p = 0.030). Conclusion:
Follow-up care in ACHD patients is often inadequate, affected by socioeconomic and behavioral factors. Smoking, lack of insurance, and relationship status are associated with a lower likelihood of follow-up. Interactions between smoking, alcohol use, and relationship status complicate their effects. Findings highlight the need for multidisciplinary interventions, including patient education, social support, and care navigation, to enhance engagement and outcomes in the ACHD population.
Adults with congenital heart disease (ACHD) are surviving longer due to medical advancements, but remain at risk for complications like heart failure and sudden cardiac death. Lifelong follow-up in specialized clinics is critical, though adherence is often low. Socioeconomic status (SES) is known to influence healthcare access; however, its impact on ACHD populations remains understudied. Understanding SES barriers to clinic attendance could inform strategies to enhance outcomes in this group.
Hypothesis:
We investigated whether SES indicators—smoking, alcohol use, drug use, marital status, employment, and insurance—predict clinic follow-up among ACHD patients. We hypothesized that socioeconomic factors would significantly influence adherence to follow-up.
Methods:
A retrospective analysis was conducted on 2,069 adults with ACHD using electronic health records from a single academic health system. The primary outcome was attendance at one follow-up visit at the ACHD clinic (Yes/No). Predictor variables were binarized for analysis. Logistic regression models were used to assess both unadjusted and adjusted associations, with interaction terms evaluated based on theoretical rationale. Model fit was assessed using AIC, lack-of-fit tests, and multicollinearity diagnostics.
Results:
Out of 2,069 patients, only 463 (22.4%) attended follow-up. In adjusted models, non-smokers had greater odds of follow-up (OR 0.49; 95% CI: 0.36–0.66; p < 0.0001). Patients without partners were more likely to follow up than those in relationships (OR 0.39; 95% CI: 0.29–0.52; p < 0.0001). Insurance coverage correlated positively with follow-up (OR 1.45; 95% CI: 1.08–1.95; p = 0.015). Drug use, alcohol use, and employment were not independently linked to follow-up, but significant interaction effects were found between smoking and alcohol use (p = 0.009) and smoking and marital status (p = 0.030). Conclusion:
Follow-up care in ACHD patients is often inadequate, affected by socioeconomic and behavioral factors. Smoking, lack of insurance, and relationship status are associated with a lower likelihood of follow-up. Interactions between smoking, alcohol use, and relationship status complicate their effects. Findings highlight the need for multidisciplinary interventions, including patient education, social support, and care navigation, to enhance engagement and outcomes in the ACHD population.
More abstracts on this topic:
3-Minute Heart Health App: A Feasibility Study
Abdulkarim Iya, Metzger Joseph, Stovitz Steven, Van't Hof Jeremy
Afterschool Rx: A Feasibility Study of a Community-Based Prescription for Reducing Cardiovascular RiskVon Klinggraeff Lauren, Beets Michael, Lane Abbi, Garimella Sudha, Armstrong Bridget, Parker Hannah, Patel Isha, Smith Michal, Coughlin Steven, Davis Catherine, Estabrooks Paul, Harris Ryan, Vernon Marlo