Final ID: Su3065
Longitudinal Left Atrial Volume Progression is Associated with Adverse Outcomes Independent of Septal Hypertrophy in Pediatric Hypertrophic Cardiomyopathy
Abstract Body (Do not enter title and authors here): Background: Baseline echocardiographic markers of diastolic dysfunction (DD), including maximum left atrial indexed volume (LAVi) and the ratio of early diastolic mitral inflow velocity to the early tissue Doppler velocity (E/e’), are associated with adverse events in pediatric hypertrophic cardiomyopathy (HCM). How these markers change over time and interact with clinical severity remains unclear.
Research Question: We aimed to assess the progression and interaction of LAVi and E/e’ with adverse clinical outcomes in children with HCM.
Methods: We conducted a single center, nested, case-control study in patients <18 years at time of HCM diagnosis. Cases developed the composite outcome of death, transplant, aborted sudden cardiac death (ASCD), sustained ventricular tachycardia (VT), myectomy or implantable cardiac defibrillator (ICD) insertion. Controls (HCM patients who did not develop composite outcome) were identified with 1:1 propensity score matching on age, sex, and septal hypertrophy. Echo DD parameters were collected at initial study and at last study defined as the study prior to event or at 5 years from initial study. Clinical outcome included transplant, sustained VT, ASCD, death; intervention outcomes included myectomy or ICD insertion. Multivariable regression modeling was performed.
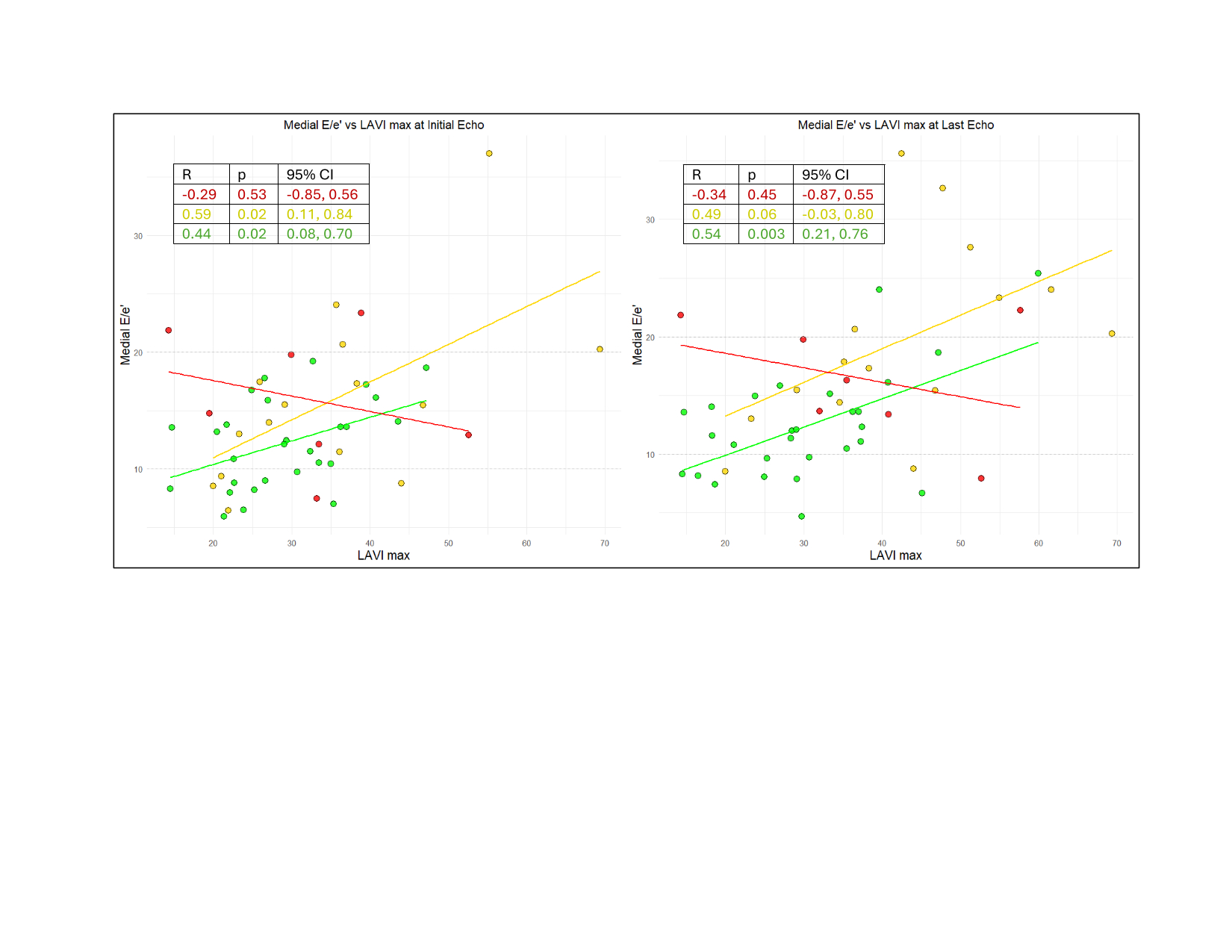
Results: The study included 98 patients (51 cases, 47 controls) with a median age of 13.9 (IQR 9.6 - 16.5). Patients experienced ICD insertion (29), myectomy (7), both ICD and myectomy (2), transplant (5), sustained ventricular tachycardia (1), ASCD (4), and death (3). LAVi was correlated with medial E/e’ in controls with intervention outcomes, but not in clinical outcomes (Figure 2). First study E/e’ medial was associated with adverse events, but association was negated when adjusted for septal wall thickness z-score (overall model p-value=0.04, E/e’ adjusted p-value=0.13). Meanwhile, LAVi was significantly associated with outcome status, independent of septal wall thickness z-score, and this association was conserved over time (initial study overall model p-value=0.013, LAVi adjusted p-value=0.016; last study overall p-value=0.004; LAVi adjusted p-value=0.009).
Conclusions: LAVi in pediatric HCM associates with outcomes independent of septal hypertrophy. LAVi appears to be a more sensitive biomarker for adverse events compared to E/e’. Future studies should explore progression of parameters of LA function as a sensitive biomarker for adverse events in pediatric HCM.
Research Question: We aimed to assess the progression and interaction of LAVi and E/e’ with adverse clinical outcomes in children with HCM.
Methods: We conducted a single center, nested, case-control study in patients <18 years at time of HCM diagnosis. Cases developed the composite outcome of death, transplant, aborted sudden cardiac death (ASCD), sustained ventricular tachycardia (VT), myectomy or implantable cardiac defibrillator (ICD) insertion. Controls (HCM patients who did not develop composite outcome) were identified with 1:1 propensity score matching on age, sex, and septal hypertrophy. Echo DD parameters were collected at initial study and at last study defined as the study prior to event or at 5 years from initial study. Clinical outcome included transplant, sustained VT, ASCD, death; intervention outcomes included myectomy or ICD insertion. Multivariable regression modeling was performed.
Results: The study included 98 patients (51 cases, 47 controls) with a median age of 13.9 (IQR 9.6 - 16.5). Patients experienced ICD insertion (29), myectomy (7), both ICD and myectomy (2), transplant (5), sustained ventricular tachycardia (1), ASCD (4), and death (3). LAVi was correlated with medial E/e’ in controls with intervention outcomes, but not in clinical outcomes (Figure 2). First study E/e’ medial was associated with adverse events, but association was negated when adjusted for septal wall thickness z-score (overall model p-value=0.04, E/e’ adjusted p-value=0.13). Meanwhile, LAVi was significantly associated with outcome status, independent of septal wall thickness z-score, and this association was conserved over time (initial study overall model p-value=0.013, LAVi adjusted p-value=0.016; last study overall p-value=0.004; LAVi adjusted p-value=0.009).
Conclusions: LAVi in pediatric HCM associates with outcomes independent of septal hypertrophy. LAVi appears to be a more sensitive biomarker for adverse events compared to E/e’. Future studies should explore progression of parameters of LA function as a sensitive biomarker for adverse events in pediatric HCM.
More abstracts on this topic:
A Diagnosis Dilemma of Positional Hypoxia: Scoliosis-Mediated Platypnea-Orthodeoxia Syndrome
Ademuwagun Christianah, Arjoon Roy, Seth Paula, Chang Gene, Ibe Oby
Arterial Stiffness and Endothelial Dysfunction can be reversed with Healthy Eating in Obese Children.Duarte Mariano, Donth Leger Gimena, Aquieri Analia, Coyle Javier, Rivas Silvia, Rodriguez Cesar, Ponzo Osvaldo