Final ID: MP662
Metabolite Risk Score Predicts Sudden Death in Patients with Cardiovascular Disease and Preserved Systolic Function
Abstract Body (Do not enter title and authors here): Introduction: Sudden cardiac death (SCD) accounts for 15–20% of all deaths, and novel risk stratification tools are urgently needed to prevent the 75% of SCDs that occur in individuals without systolic dysfunction who do not qualify for primary prevention implantable cardioverter-defibrillators (ICDs).
Hypothesis: We hypothesize that disruptions in metabolic pathways may predispose to SCD in the setting of coronary heart disease (CHD) and that plasma metabolites (MTBs) may serve as novel biomarkers that, in combination, might identify patients at elevated SCD risk.
Methods: The PREDETERMINE study is an ongoing multicenter prospective cohort of patients with CHD and left ventricular ejection fraction (LVEF) > 30-35% who were not eligible for ICDs at baseline. Among 5,570 participants, 509 annotated plasma metabolites were measured using liquid chromatography-mass spectrometry (LC-MS). A metabolite risk score (MRS) was constructed using metabolites selected and effect sizes derived from age- and sex-adjusted LASSO Fine-Gray model predicting SCD, with Non-SCD treated as a competing risk outcome. Characteristics of MRS was examined using cumulative incidence curves, multivariable-adjusted Fine-Gray Cox regression, and competing risk analysis. Discrimination was evaluated via area under the curve (AUC), compared to clinical models.
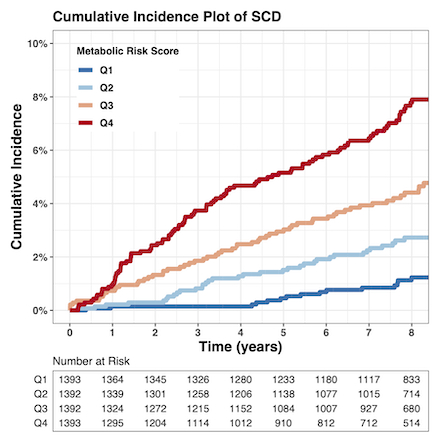
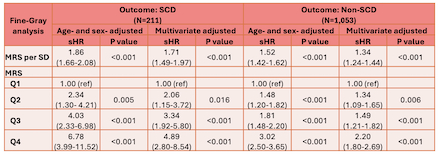
Results: Over a median 8-year follow-up, there were 211 (3.8%) SCDs and 1,053 (18.9%) non-SCDs. Twenty-two MTBs involved with more than 25 pathways spanning amino acid, lipid/steroid, and central carbon metabolism were selected to construct the MRS. At 8 years, participants in the top quartile had an unadjusted cumulative incidence of SCD of 7.8 % (95% CI: 6.4%-9.4%) compared to 1.2 % (95% CI: 0.7%-2.0%) in the bottom quartile (Figure). After multivariable adjustment for age, sex, LVEF, and other SCD risk factors, the MRS remained significantly associated with SCD (sHR per SD 1.71, 95% CI 1.49–1.97, p<0.001; sHR 4.89 for top vs bottom quartile, 95%CI, 2.80-8.54, P<0.001). The relationship of the MRS was stronger for SCD versus non-SCD (Table, P for differential <0.001). Adding MRS to multivariable models improved AUC for SCD from 70.3 % to 74.1% (P=0.004).
Conclusions: A MRS significantly improves SCD prediction in CAD patients without significant systolic dysfunction at baseline and may serve as a valuable tool for identifying high-risk individuals for targeted preventive interventions.
Hypothesis: We hypothesize that disruptions in metabolic pathways may predispose to SCD in the setting of coronary heart disease (CHD) and that plasma metabolites (MTBs) may serve as novel biomarkers that, in combination, might identify patients at elevated SCD risk.
Methods: The PREDETERMINE study is an ongoing multicenter prospective cohort of patients with CHD and left ventricular ejection fraction (LVEF) > 30-35% who were not eligible for ICDs at baseline. Among 5,570 participants, 509 annotated plasma metabolites were measured using liquid chromatography-mass spectrometry (LC-MS). A metabolite risk score (MRS) was constructed using metabolites selected and effect sizes derived from age- and sex-adjusted LASSO Fine-Gray model predicting SCD, with Non-SCD treated as a competing risk outcome. Characteristics of MRS was examined using cumulative incidence curves, multivariable-adjusted Fine-Gray Cox regression, and competing risk analysis. Discrimination was evaluated via area under the curve (AUC), compared to clinical models.
Results: Over a median 8-year follow-up, there were 211 (3.8%) SCDs and 1,053 (18.9%) non-SCDs. Twenty-two MTBs involved with more than 25 pathways spanning amino acid, lipid/steroid, and central carbon metabolism were selected to construct the MRS. At 8 years, participants in the top quartile had an unadjusted cumulative incidence of SCD of 7.8 % (95% CI: 6.4%-9.4%) compared to 1.2 % (95% CI: 0.7%-2.0%) in the bottom quartile (Figure). After multivariable adjustment for age, sex, LVEF, and other SCD risk factors, the MRS remained significantly associated with SCD (sHR per SD 1.71, 95% CI 1.49–1.97, p<0.001; sHR 4.89 for top vs bottom quartile, 95%CI, 2.80-8.54, P<0.001). The relationship of the MRS was stronger for SCD versus non-SCD (Table, P for differential <0.001). Adding MRS to multivariable models improved AUC for SCD from 70.3 % to 74.1% (P=0.004).
Conclusions: A MRS significantly improves SCD prediction in CAD patients without significant systolic dysfunction at baseline and may serve as a valuable tool for identifying high-risk individuals for targeted preventive interventions.
More abstracts on this topic:
Association of Eicosanoid Metabolites with Insulin Resistance
Parekh Juhi, Chitsazan Mandana, Roshandelpoor Athar, Alotaibi Mona, Jain Mohit, Cheng Susan, Ho Jennifer
Finerenone Reduces Sudden Death across the Spectrum of Cardio-Kidney-Metabolism: the FINE-HEART Pooled AnalysisFoa' Alberto, De Sanctis Yoriko, Lam Carolyn, Senni Michele, Shah Sanjiv, Voors Adriaan, Zannad Faiez, Rossing Peter, Ruilope Luis, Anker Stefan, Pitt Bertram, Pabon Maria, Agarwal Rajiv, Mcmurray John, Solomon Scott, Vaduganathan Muthiah, Desai Akshay, Filippatos Gerasimos, Claggett Brian, Jhund Pardeep, Henderson Alasdair David, Brinker Meike, Lage Andrea, Hofmeister Lucas