Final ID: MP413
Energy Insecurity Associates with Increased Odds of Cardiovascular Disease Risk Factors and Burden: Data from the Behavioral Risk Factor Surveillance System, 2023
Abstract Body (Do not enter title and authors here): Introduction: Over a quarter of US households experience energy insecurity (EI) - the inability to meet household energy needs - and this number is expected to rise due to increasing global temperatures and energy demands. EI has been shown to impact health due to financial tradeoffs with healthcare, but limited evidence exists on how EI may contribute to cardiovascular disease (CVD) risk factors and burden.
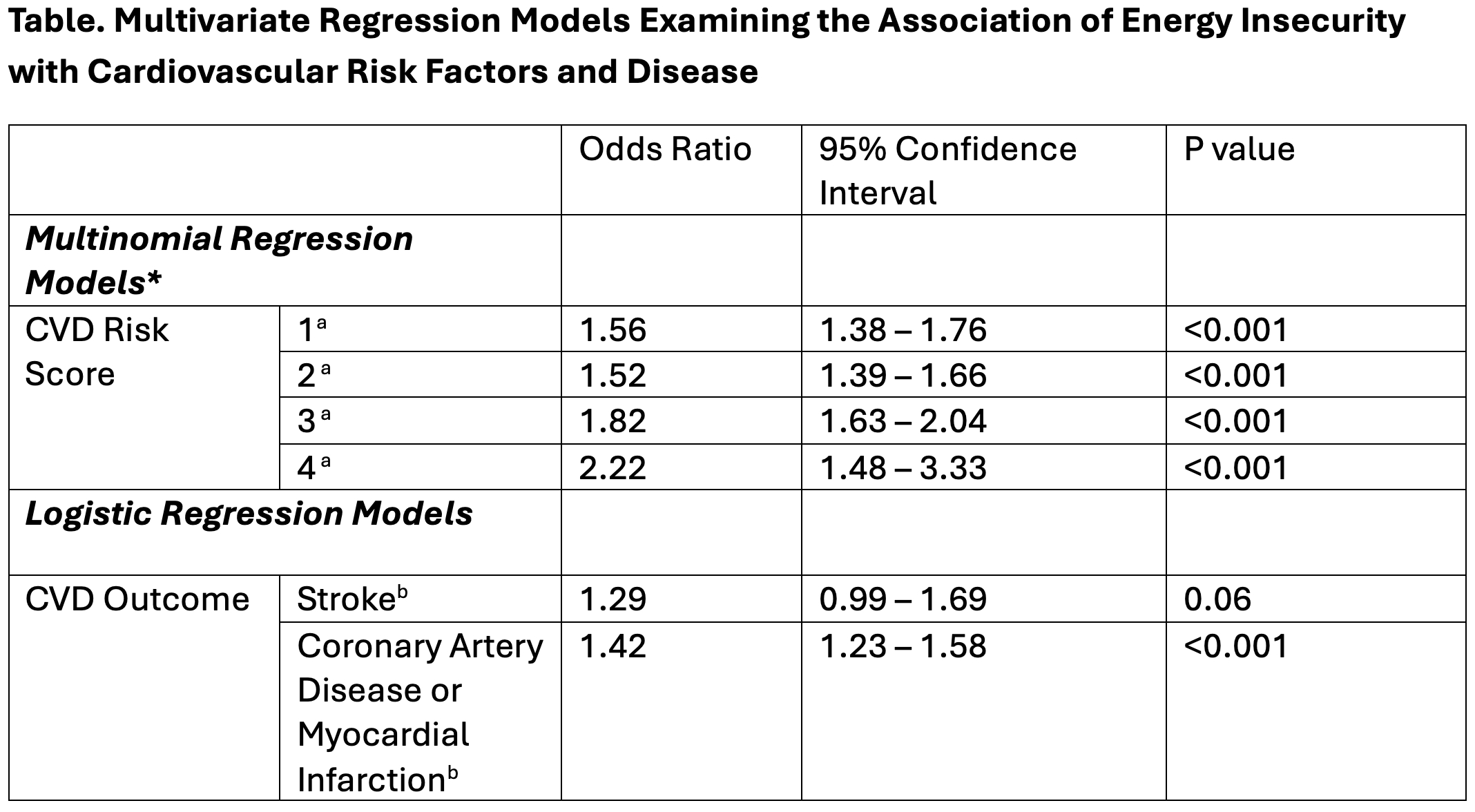
Methods: Using Behavioral Risk Factor Surveillance – a nationally representative survey – data from 2023, we examined the relationship between EI and CVD risk factors and outcomes among households with incomes at and below 200% of the federal poverty level. EI was defined as experiencing a threat of utility disconnection for electric, gas, oil or water in the past 12 months. CVD risk factors (high cholesterol, hypertension, diabetes and tobacco use) were assessed as a composite risk score (range 0 to 4) by counting the total number of conditions. We performed a complete case analysis and used weighted multinomial regression models to analyze the relationship between EI and CVD risk scores. Demographic and socioeconomic covariates were included in the model. We used logistic regression models to evaluate the relationship with CVD (coronary artery disease (CAD), myocardial infarction (MI) or stroke). CVD risk factors were also included as covariates in these models. Survey weights were used to account for the complex survey design.
Results: Within the study population (N= 53,389; 15.72% Black, 44.95% White and 28.38% Hispanic), those who reported EI (N=7,910) were found to be younger (median age: 42 (IQR 33.5) vs. 46 (IQR 31.6) years) and more likely to be female (62.5% vs. 56.7%), unemployed/unable to work (46.2% vs. 35.1%), and have public insurance (67.5% vs. 61.8%). In the adjusted model, EI was associated with significantly higher odds of reporting one or more CVD risk factors (Table) with OR of 2.22 (95% CI 1.48–3.33) for having all four risk factors. EI was also associated with higher odds of CAD or MI [1.42 (95% CI 1.23-1.58)]. There was a non-statistically significant higher odds of stroke [1.29 (95% CI 0.99-1.69)].
Conclusions: EI was associated with higher odds of CVD risk factors and burden among low-income adults. EI may be an important marker of increased risk of CVD, possibly due to financial tradeoffs, impaired healthcare access and management, or stress related physiologic pathways.
Methods: Using Behavioral Risk Factor Surveillance – a nationally representative survey – data from 2023, we examined the relationship between EI and CVD risk factors and outcomes among households with incomes at and below 200% of the federal poverty level. EI was defined as experiencing a threat of utility disconnection for electric, gas, oil or water in the past 12 months. CVD risk factors (high cholesterol, hypertension, diabetes and tobacco use) were assessed as a composite risk score (range 0 to 4) by counting the total number of conditions. We performed a complete case analysis and used weighted multinomial regression models to analyze the relationship between EI and CVD risk scores. Demographic and socioeconomic covariates were included in the model. We used logistic regression models to evaluate the relationship with CVD (coronary artery disease (CAD), myocardial infarction (MI) or stroke). CVD risk factors were also included as covariates in these models. Survey weights were used to account for the complex survey design.
Results: Within the study population (N= 53,389; 15.72% Black, 44.95% White and 28.38% Hispanic), those who reported EI (N=7,910) were found to be younger (median age: 42 (IQR 33.5) vs. 46 (IQR 31.6) years) and more likely to be female (62.5% vs. 56.7%), unemployed/unable to work (46.2% vs. 35.1%), and have public insurance (67.5% vs. 61.8%). In the adjusted model, EI was associated with significantly higher odds of reporting one or more CVD risk factors (Table) with OR of 2.22 (95% CI 1.48–3.33) for having all four risk factors. EI was also associated with higher odds of CAD or MI [1.42 (95% CI 1.23-1.58)]. There was a non-statistically significant higher odds of stroke [1.29 (95% CI 0.99-1.69)].
Conclusions: EI was associated with higher odds of CVD risk factors and burden among low-income adults. EI may be an important marker of increased risk of CVD, possibly due to financial tradeoffs, impaired healthcare access and management, or stress related physiologic pathways.
More abstracts on this topic:
An Evaluation of Bystander CPR by Race, Accounting for Social Drivers of Health
Lane Nina, Crowe Remle, Salcido David
Age-stratified Monogenic and Polygenic Contributions for Atrial Fibrillation in the All of Us Research ProgramChen Zhanlin, Gordon Adam, Webster Gregory