Final ID: MP2426
Genetic Evaluation of Familial Hypercholesterolemia in a Pediatric Cardiology Clinic
Abstract Body (Do not enter title and authors here): Background: Familial hypercholesterolemia (FH) is an autosomal dominant disorder characterized by elevated low density lipoprotein cholesterol (LDL-C) and increased lifetime risk of atherosclerotic cardiovascular disease (ASCVD). While clinical criteria have been established to diagnose FH, genetic testing is now widely available providing an additional avenue for diagnosis. We aimed to describe the yield of genetic testing for FH in children evaluated in a dedicated pediatric cardiology clinic.
Methods: We conducted a retrospective cohort study based on the initial evaluation of children in a dyslipidemia clinic between 2017 and 2024. Genetic testing for FH was performed based on assessment of clinical criteria by the attending preventive cardiologist. The cohort was divided into three categories based on genetic testing: genotype positive, genotype negative and phenotype negative (genetic testing not ordered). Patient characteristics and lab parameters (fasting LDL-C and triglycerides, and lipoprotein(a) in mg/dL) were compared between the three groups using descriptive statistics, chi-squared, or Kruskal-Wallis tests.
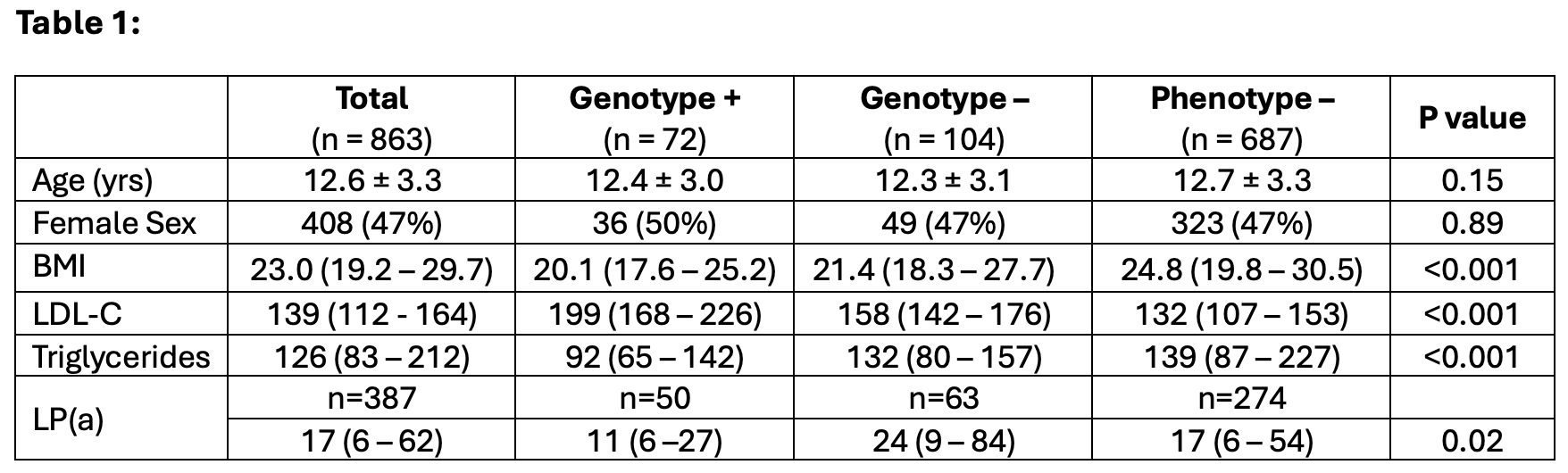
Results: Of 863 pediatric patients evaluated (47% female, mean age 12.6 ± 3.3 years) genetic testing was performed in 176 probands. A pathogenic or likely pathogenic variant was identified in 72 (41%) including 58 LDLR (81%), 12 APOB (17%), 2 PCSK9 (2%) variants. Data are summarized in Table 1. The genotype positive cohort had higher LDL-C compared to the phenotype negative and genotype negative cohorts. Genotype negative patients had higher lipoprotein (a). The phenotype negative group had higher triglyceride levels and BMI. An additional 304 patients (164 adult patients) underwent cascade family screening that yielded 169 patients (87 adult patients) with pathogenic or likely pathogenic variants (137 LDLR [81.5%], 31 APOB [18%], 1 PCSK9 [0.5%]).
Conclusion: The diagnostic yield of genetic testing to confirm FH in clinically suspected pediatric patients is high and enables effective cascade screening. Lipoprotein (a) should be considered in all patients, especially those with negative FH genetic testing. Systematic implementation of pediatric lipid screening and targeted genetic testing may enhance early diagnosis of FH in children and family members, enabling timely interventions in this high-risk cohort.
Methods: We conducted a retrospective cohort study based on the initial evaluation of children in a dyslipidemia clinic between 2017 and 2024. Genetic testing for FH was performed based on assessment of clinical criteria by the attending preventive cardiologist. The cohort was divided into three categories based on genetic testing: genotype positive, genotype negative and phenotype negative (genetic testing not ordered). Patient characteristics and lab parameters (fasting LDL-C and triglycerides, and lipoprotein(a) in mg/dL) were compared between the three groups using descriptive statistics, chi-squared, or Kruskal-Wallis tests.
Results: Of 863 pediatric patients evaluated (47% female, mean age 12.6 ± 3.3 years) genetic testing was performed in 176 probands. A pathogenic or likely pathogenic variant was identified in 72 (41%) including 58 LDLR (81%), 12 APOB (17%), 2 PCSK9 (2%) variants. Data are summarized in Table 1. The genotype positive cohort had higher LDL-C compared to the phenotype negative and genotype negative cohorts. Genotype negative patients had higher lipoprotein (a). The phenotype negative group had higher triglyceride levels and BMI. An additional 304 patients (164 adult patients) underwent cascade family screening that yielded 169 patients (87 adult patients) with pathogenic or likely pathogenic variants (137 LDLR [81.5%], 31 APOB [18%], 1 PCSK9 [0.5%]).
Conclusion: The diagnostic yield of genetic testing to confirm FH in clinically suspected pediatric patients is high and enables effective cascade screening. Lipoprotein (a) should be considered in all patients, especially those with negative FH genetic testing. Systematic implementation of pediatric lipid screening and targeted genetic testing may enhance early diagnosis of FH in children and family members, enabling timely interventions in this high-risk cohort.
More abstracts on this topic:
A Novel Variant in GNB2 as a Cause of Sick Sinus Syndrome
Bulut Aybike, Karacan Mehmet, Saygili E. Alper, Pirli Dogukan, Aydin Eylul, Ozdemir Ozkan, Balci Nermin, Alanay Yasemin, Bilguvar Kaya, Akgun Dogan Ozlem
Adiponectin and Adiponectin/Leptin Ratio Associate with Cardiometabolic Risk in South Asian Americans: Updates from the MASALA StudyUttarwar Salil, Shah Nilay, Kanaya Alka, Gadgil Meghana