Final ID: MP1513
Artificial Intelligence–Enabled Electrocardiography for Detecting Risk of Rehospitalization in patients with Heart Failure
Abstract Body (Do not enter title and authors here): Background
Preventing and managing hospital readmissions is critical in heart failure (HF) care, yet conventional monitoring tools have limitations. While artificial intelligence-enabled electrocardiograms (AI-ECGs) show promise in detecting cardiac dysfunction, little is known about their post-discharge score dynamics in HF patients.
Hypothesize
We hypothesized that AI-enabled ECG scores would show distinct temporal patterns after hospital discharge in patients with HF, and that these patterns would differ between patients who experienced rehospitalization and those who did not.
Method
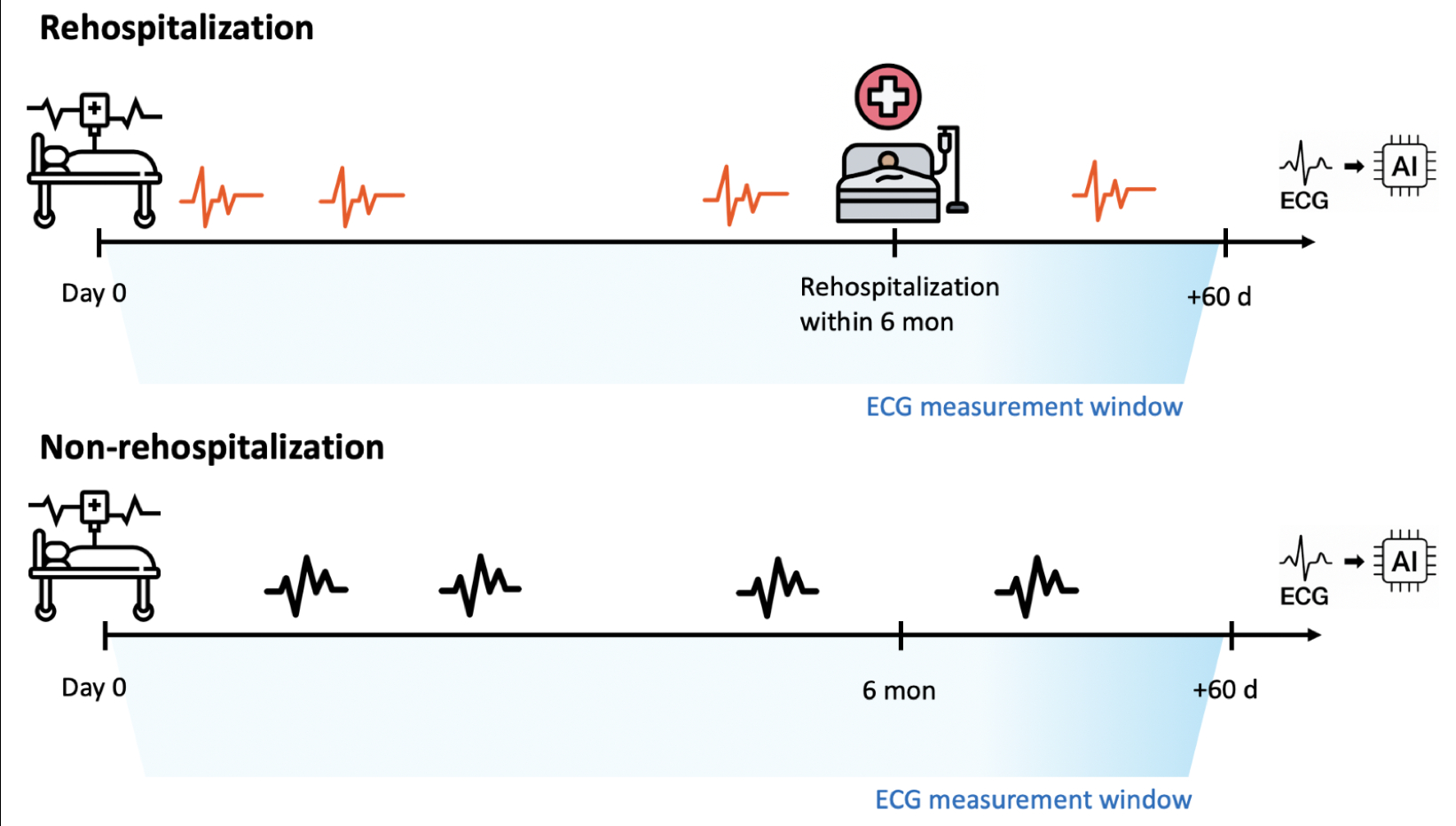
This single-center retrospective study analyzed ECG data from patients hospitalized for HF between March 2017 and January 2025 in South Korea. Post-discharge, ECGs were processed using AI-ECG models for left ventricular systolic dysfunction (LVSD), diastolic dysfunction (LVDD), and myocardial infarction (MI). We compared AI-ECG patterns in patients readmitted within six months vs. those not (Figure 1). Temporal trends in AI-ECG scores were assessed using a mixed-effects linear regression model with group and time as fixed effects, and patient as a random effect.
Result
Among 1,007 patients, 1,539 hospitalization events were identified. A total of 1,674 ECGs from 269 rehospitalized and 4,066 ECGs from 917 non-rehospitalized patients were collected from 180 days before to 60 days after the index readmission or follow-up end. The mean age was 65.2 years, and 63.1% were male. Diabetes mellitus and chronic kidney disease were significantly more prevalent in the rehospitalization group, whereas other comorbidities were comparable. Significant differences in ECG intervals and axes were also observed, with no notable difference in heart rate.
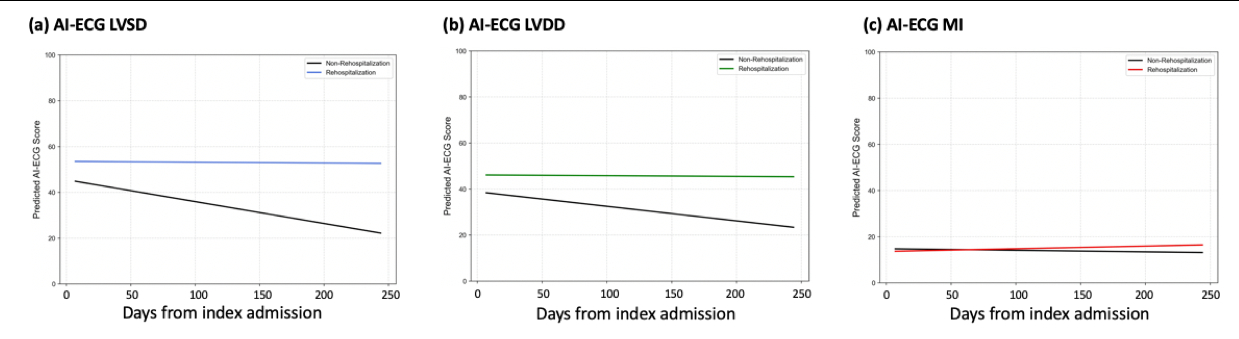
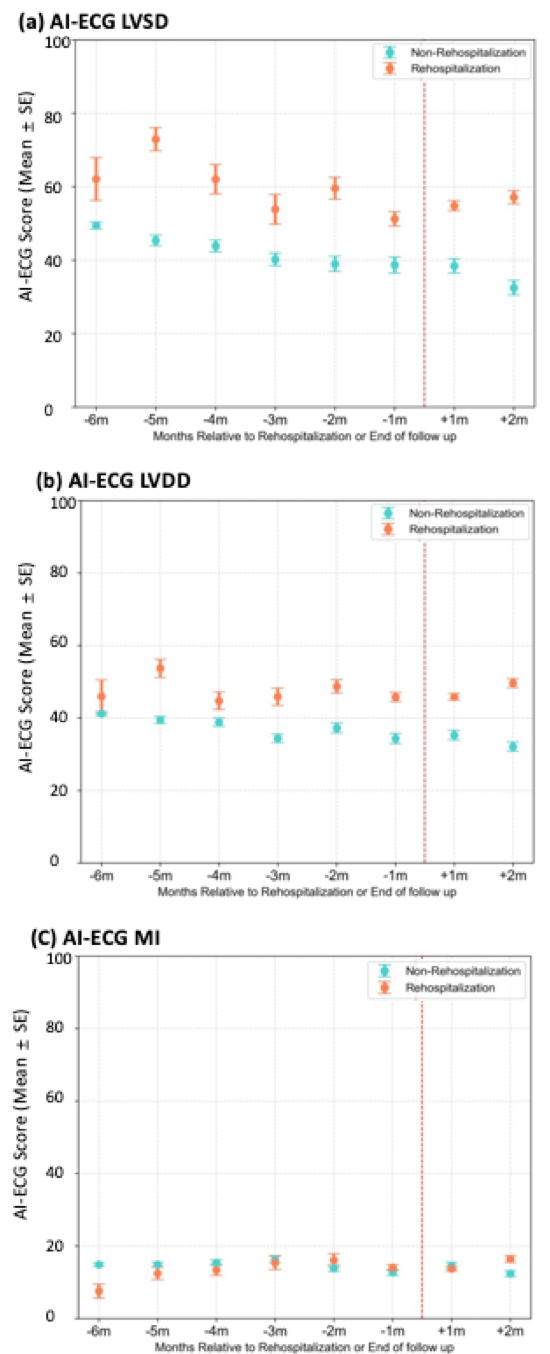
In the LVSD model, rehospitalized patients showed higher scores overall (β = 7.96, 95% CI: 3.18–12.75, p = 0.001) (Figure 2). Time since discharge was associated with decreasing scores (β = –0.096/day, 95% CI: –0.104 to –0.087, p<0.001), but this decline was attenuated in the rehospitalization group (interaction β = 0.092, 95% CI: 0.069–0.115, p<0.001). The LVDD model demonstrated a similar trend, while the MI model exhibited no statistically significant differences in scores (Figure 3).
Conclusion
AI-ECG models show potential as dynamic biomarkers for detecting early physiological deterioration and predicting readmission risk in HF patients. These findings support their use in future patient monitoring strategies.
Preventing and managing hospital readmissions is critical in heart failure (HF) care, yet conventional monitoring tools have limitations. While artificial intelligence-enabled electrocardiograms (AI-ECGs) show promise in detecting cardiac dysfunction, little is known about their post-discharge score dynamics in HF patients.
Hypothesize
We hypothesized that AI-enabled ECG scores would show distinct temporal patterns after hospital discharge in patients with HF, and that these patterns would differ between patients who experienced rehospitalization and those who did not.
Method
This single-center retrospective study analyzed ECG data from patients hospitalized for HF between March 2017 and January 2025 in South Korea. Post-discharge, ECGs were processed using AI-ECG models for left ventricular systolic dysfunction (LVSD), diastolic dysfunction (LVDD), and myocardial infarction (MI). We compared AI-ECG patterns in patients readmitted within six months vs. those not (Figure 1). Temporal trends in AI-ECG scores were assessed using a mixed-effects linear regression model with group and time as fixed effects, and patient as a random effect.
Result
Among 1,007 patients, 1,539 hospitalization events were identified. A total of 1,674 ECGs from 269 rehospitalized and 4,066 ECGs from 917 non-rehospitalized patients were collected from 180 days before to 60 days after the index readmission or follow-up end. The mean age was 65.2 years, and 63.1% were male. Diabetes mellitus and chronic kidney disease were significantly more prevalent in the rehospitalization group, whereas other comorbidities were comparable. Significant differences in ECG intervals and axes were also observed, with no notable difference in heart rate.
In the LVSD model, rehospitalized patients showed higher scores overall (β = 7.96, 95% CI: 3.18–12.75, p = 0.001) (Figure 2). Time since discharge was associated with decreasing scores (β = –0.096/day, 95% CI: –0.104 to –0.087, p<0.001), but this decline was attenuated in the rehospitalization group (interaction β = 0.092, 95% CI: 0.069–0.115, p<0.001). The LVDD model demonstrated a similar trend, while the MI model exhibited no statistically significant differences in scores (Figure 3).
Conclusion
AI-ECG models show potential as dynamic biomarkers for detecting early physiological deterioration and predicting readmission risk in HF patients. These findings support their use in future patient monitoring strategies.
More abstracts on this topic:
A Scoping Review Exploring Cardiovascular Risk and Health Metrics and Cancer Prediction
Kim Ji-eun, Henriquez Santos Gretell, Kumar Sant, Livinski Alicia, Vo Jacqueline, Joo Jungnam, Shearer Joe, Hashemian Maryam, Roger Veronique
A Machine Learning Algorithm to Detect Pediatric Supraventricular Tachycardia Risk from Baseline ECGsArezoumand Amirhossein, Danala Gopichandh, Masnadi Khiabani Parisa, Ebert David, Behere Shashank