Final ID: MP2556
Management of Mechanical Mitral Valve Thrombosis Using Multimodal Imaging and Thrombolysis
Abstract Body (Do not enter title and authors here):
Case Description
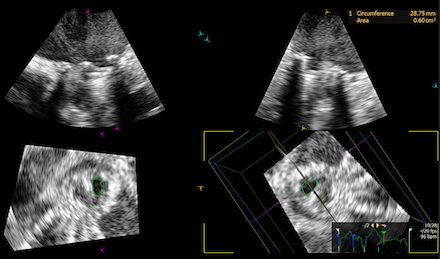
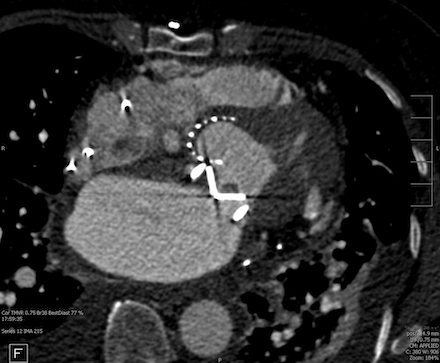
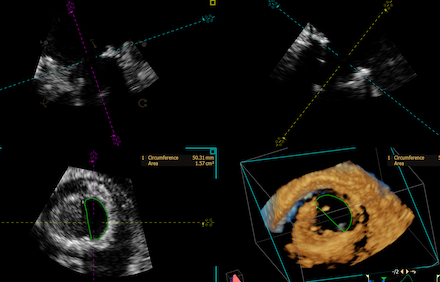
A 66 year old female with past medical history of rheumatic heart disease requiring mechanical mitral valve (MV) replacement on warfarin, HFpEF (EF 60%), atrial fibrillation requiring dual chamber pacemaker presented with worsening dyspnea on exertion. The patient was admitted for acute on chronic heart failure exacerbation requiring diuresis. Transthoracic echocardiogram (TTE) revealed significantly elevated gradients across the mitral prosthesis, concerning for significant prosthetic stenosis (peak velocity 2.4 m/s and mean gradient of 14 mmHg). Transesophageal echocardiogram (TEE) demonstrated moderate to severe mitral stenosis with a valve area of 0.6 sq cm by 3D planimetry, and poor leaflet excursion concerning for thrombus or pannus (Figure 1). Cardiac CT was suggestive of thrombus around the mechanical MV leaflets (Figure 2). Clinically, the patient had interval worsening heart failure symptoms and chest x-ray with worsening pulmonary edema. After consultation with cardiothoracic surgery, tPA was administered over 24 hours under close monitoring in the Cardiac Critical Care Unit. Repeat TEE post-thrombolysis showed improvement in MV area to 1.57 sq cm by 3D planimetry, with increased mobility of one mechanical MV leaflet (Figure 3). Persistent restriction of the other leaflet concerning for pannus remained, with no urgent surgical intervention indicated.
Methods/Methodology
Multimodal imaging, including TTE, TEE with 3D planimetry, and cardiac CT, guided diagnosis. Management involved low-dose, prolonged-infusion thrombolysis for a stable patient at high surgical risk. Clinical and imaging responses were monitored to guide further treatment decisions.
Discussion
Mechanical valve thrombosis management is a serious complication that can be caused by subtherapeutic anticoagulation or poor medication adherence. Management is guided by symptom severity, thrombus size, and surgical risk. Surgery can provide definitive treatment, but carries high risk, especially in unstable or comorbid patients. Thrombolytic therapy offers a less invasive option and is often preferred for stable patients (NYHA class I-III) with small thrombi and high surgical risk. Protocols utilizing low dose, slow infusion thrombolytics are associated with improved safety outcomes. Echocardiography is essential for diagnosis and monitoring response to therapy. A multidisciplinary approach along with close follow up and INR monitoring helps prevent recurrence.
Case Description
A 66 year old female with past medical history of rheumatic heart disease requiring mechanical mitral valve (MV) replacement on warfarin, HFpEF (EF 60%), atrial fibrillation requiring dual chamber pacemaker presented with worsening dyspnea on exertion. The patient was admitted for acute on chronic heart failure exacerbation requiring diuresis. Transthoracic echocardiogram (TTE) revealed significantly elevated gradients across the mitral prosthesis, concerning for significant prosthetic stenosis (peak velocity 2.4 m/s and mean gradient of 14 mmHg). Transesophageal echocardiogram (TEE) demonstrated moderate to severe mitral stenosis with a valve area of 0.6 sq cm by 3D planimetry, and poor leaflet excursion concerning for thrombus or pannus (Figure 1). Cardiac CT was suggestive of thrombus around the mechanical MV leaflets (Figure 2). Clinically, the patient had interval worsening heart failure symptoms and chest x-ray with worsening pulmonary edema. After consultation with cardiothoracic surgery, tPA was administered over 24 hours under close monitoring in the Cardiac Critical Care Unit. Repeat TEE post-thrombolysis showed improvement in MV area to 1.57 sq cm by 3D planimetry, with increased mobility of one mechanical MV leaflet (Figure 3). Persistent restriction of the other leaflet concerning for pannus remained, with no urgent surgical intervention indicated.
Methods/Methodology
Multimodal imaging, including TTE, TEE with 3D planimetry, and cardiac CT, guided diagnosis. Management involved low-dose, prolonged-infusion thrombolysis for a stable patient at high surgical risk. Clinical and imaging responses were monitored to guide further treatment decisions.
Discussion
Mechanical valve thrombosis management is a serious complication that can be caused by subtherapeutic anticoagulation or poor medication adherence. Management is guided by symptom severity, thrombus size, and surgical risk. Surgery can provide definitive treatment, but carries high risk, especially in unstable or comorbid patients. Thrombolytic therapy offers a less invasive option and is often preferred for stable patients (NYHA class I-III) with small thrombi and high surgical risk. Protocols utilizing low dose, slow infusion thrombolytics are associated with improved safety outcomes. Echocardiography is essential for diagnosis and monitoring response to therapy. A multidisciplinary approach along with close follow up and INR monitoring helps prevent recurrence.
More abstracts on this topic:
A Rare Case of Epicardial Cavernous Hemangioma with Coexisting Severe Mitral Regurgitation
Abdallah Ala, Sutton Jenna, Houshmand Nazanin, Gupta Neelesh, Ahsan Chowdhury
A Rare Case Of Localized Ventricular Tachycardia Due To Mitral Annular Disjunction And a Subvalvular AneurysmO'toole Timothy, Binder Michael, Hama Amin Ali