Final ID: MP1328
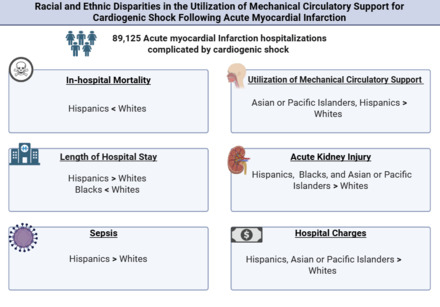
Racial and Ethnic Disparities in the Utilization of Mechanical Circulatory Support for Cardiogenic Shock Following Acute Myocardial Infarction
Abstract Body (Do not enter title and authors here): Background: Cardiogenic shock (CS) complicating acute myocardial infarction (AMI) carries high morbidity and mortality. Mechanical circulatory support (MCS) devices are critical in management, but racial and ethnic disparities in MCS utilization remain understudied.
Research Question: Do disparities exist in the utilization of MCS and healthcare resources among racial and ethnic groups with AMI-CS in the United States?
Methods: We extracted data from the National Inpatient Sample database from 2018 to 2020. We included patients aged ≥18 years with AMI and CS listed as primary or secondary diagnosis, identified using ICD-10-CM (AMI: I21.0–I21.4; CS: R57.0). Racial/ethnic groups analyzed included White, Black, Hispanic, and Asian or Pacific Islander. The primary outcome was in-hospital mortality. Secondary outcomes included MCS utilization, hospital length of stay (LOS), total hospital charges, acute kidney injury (AKI)/hemodialysis, and sepsis. Multivariable logistic and linear regression models were used to assess associations between race/ethnicity and in-hospital outcomes, adjusting for potential covariates.
Results: Among 89,125 hospitalizations for AMI-CS, Hispanic individuals had lower odds of in-hospital mortality compared to White individuals (OR 0.86; 95% CI, 0.76–0.96), while no significant differences were observed for other racial and ethnic groups. The odds of receiving MCS were higher among Asian or Pacific Islander (OR 1.35; 95% CI, 1.14–1.60) and Hispanic individuals (OR 1.15; 95% CI, 1.01–1.30) relative to White individuals. Compared to White individuals, Hispanic individuals had longer hospital stays (β = 1.3 days; 95% CI, 0.78–1.7), whereas Black individuals had shorter stays (β = –0.50 days; 95% CI, –0.91 - –0.10). The odds of AKI or hemodialysis were higher in Hispanic (OR 1.26; 95% CI, 1.12–1.42), Black (OR 1.59; 95% CI, 1.40–1.79), and Asian or Pacific Islander individuals (OR 1.39; 95% CI, 1.18–1.64) compared to White individuals. Hispanic individuals also had higher odds of developing sepsis (OR 1.18; 95% CI, 1.04–1.34). Additionally, total hospital charges were significantly greater for Hispanic ($53,770; 95% CI, $39,307–$68,233) and Asian or Pacific Islander individuals ($33,737; 95% CI, $8,954–$58,520) compared to White individuals.
Conclusion: Racial and ethnic disparities in MCS use and clinical outcomes persist among patients with AMI and CS, highlighting the need for targeted strategies to improve AMI care.
Research Question: Do disparities exist in the utilization of MCS and healthcare resources among racial and ethnic groups with AMI-CS in the United States?
Methods: We extracted data from the National Inpatient Sample database from 2018 to 2020. We included patients aged ≥18 years with AMI and CS listed as primary or secondary diagnosis, identified using ICD-10-CM (AMI: I21.0–I21.4; CS: R57.0). Racial/ethnic groups analyzed included White, Black, Hispanic, and Asian or Pacific Islander. The primary outcome was in-hospital mortality. Secondary outcomes included MCS utilization, hospital length of stay (LOS), total hospital charges, acute kidney injury (AKI)/hemodialysis, and sepsis. Multivariable logistic and linear regression models were used to assess associations between race/ethnicity and in-hospital outcomes, adjusting for potential covariates.
Results: Among 89,125 hospitalizations for AMI-CS, Hispanic individuals had lower odds of in-hospital mortality compared to White individuals (OR 0.86; 95% CI, 0.76–0.96), while no significant differences were observed for other racial and ethnic groups. The odds of receiving MCS were higher among Asian or Pacific Islander (OR 1.35; 95% CI, 1.14–1.60) and Hispanic individuals (OR 1.15; 95% CI, 1.01–1.30) relative to White individuals. Compared to White individuals, Hispanic individuals had longer hospital stays (β = 1.3 days; 95% CI, 0.78–1.7), whereas Black individuals had shorter stays (β = –0.50 days; 95% CI, –0.91 - –0.10). The odds of AKI or hemodialysis were higher in Hispanic (OR 1.26; 95% CI, 1.12–1.42), Black (OR 1.59; 95% CI, 1.40–1.79), and Asian or Pacific Islander individuals (OR 1.39; 95% CI, 1.18–1.64) compared to White individuals. Hispanic individuals also had higher odds of developing sepsis (OR 1.18; 95% CI, 1.04–1.34). Additionally, total hospital charges were significantly greater for Hispanic ($53,770; 95% CI, $39,307–$68,233) and Asian or Pacific Islander individuals ($33,737; 95% CI, $8,954–$58,520) compared to White individuals.
Conclusion: Racial and ethnic disparities in MCS use and clinical outcomes persist among patients with AMI and CS, highlighting the need for targeted strategies to improve AMI care.
More abstracts on this topic:
A Machine Learning-Derived Socio-Environmental Risk Score More Accurately Predicts Cardiovascular Events and Better Addresses Health Inequities than Social Deprivation Index
Chen Zhuo, Nasir Khurram, Al-kindi Sadeer, Rajagopalan Sanjay, Ponnana Sai Rahul, Dazard Jean-eudes, Zhang Tong, Dong Weichuan, Okyere Robert, Sirasapalli Santosh, Deo Salil, Khraishah Haitham
A Systematic Review and Meta-Analysis on the Anesthetic Approaches for Left Atrial Appendage Occlusion: Comparing Conscious Sedation and General AnesthesiaZaidi Syed Rafay, Ajmal Umna, Rauf Zainab, Maaz Muhammad, Gulzar Sara, Burki Shahid, Nazir Abubakar, Mirza Azka, Hassan Ahmad, Amir Maaz, Jahangir Muhammad Asad, Rasul Minahil, Raza Muhammad, Malik Mohammad