Final ID: Mo2057
Effects of Gender on Outcomes in Acute Type A Aortic Dissection
Abstract Body (Do not enter title and authors here): Objective: Although gender-related disparities in cardiovascular surgery have been investigated extensively in the past decades, knowledge about the impact of gender on outcomes after surgery for acute aortic dissection type A (AADA) is sparse. The aim of this study was to compare differences in presentation, treatment, and outcome in female and male patients with acute type A aortic dissection.
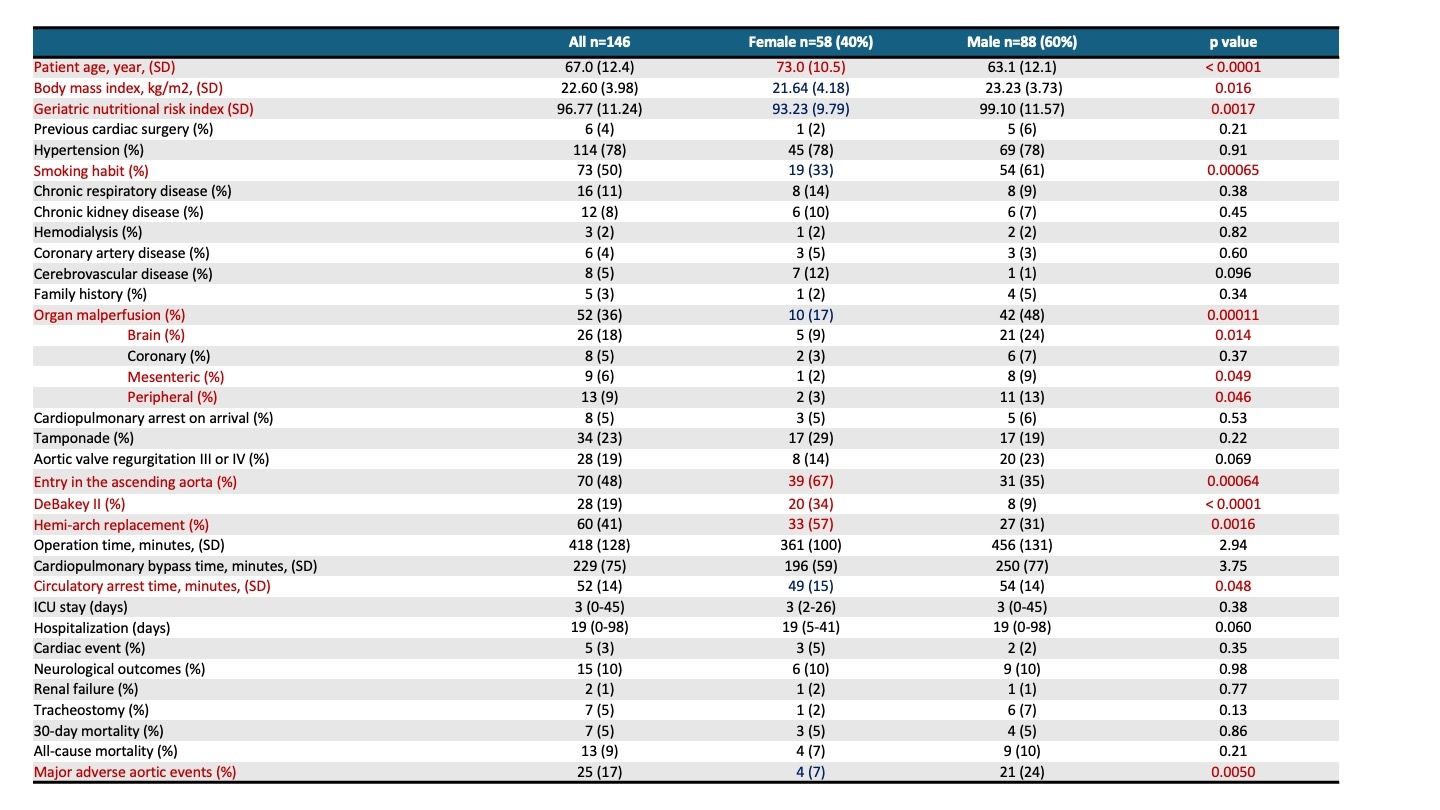
Methods: From September 2015 to December 2023, 146 patients, consisting of 58 women and 88 men, underwent surgery for acute type A aortic dissection at our institution. We compared clinical features and events between the 2 cohorts.
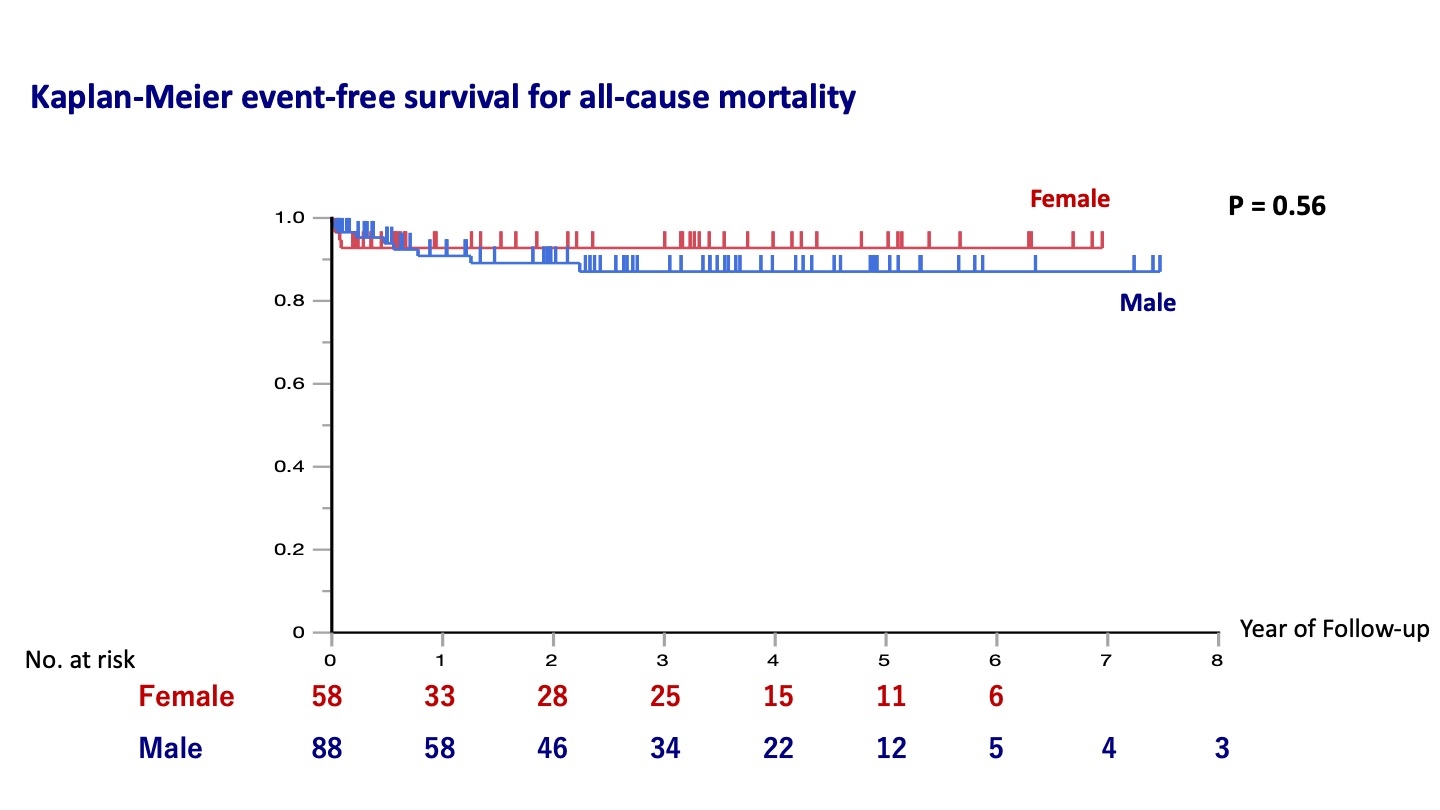
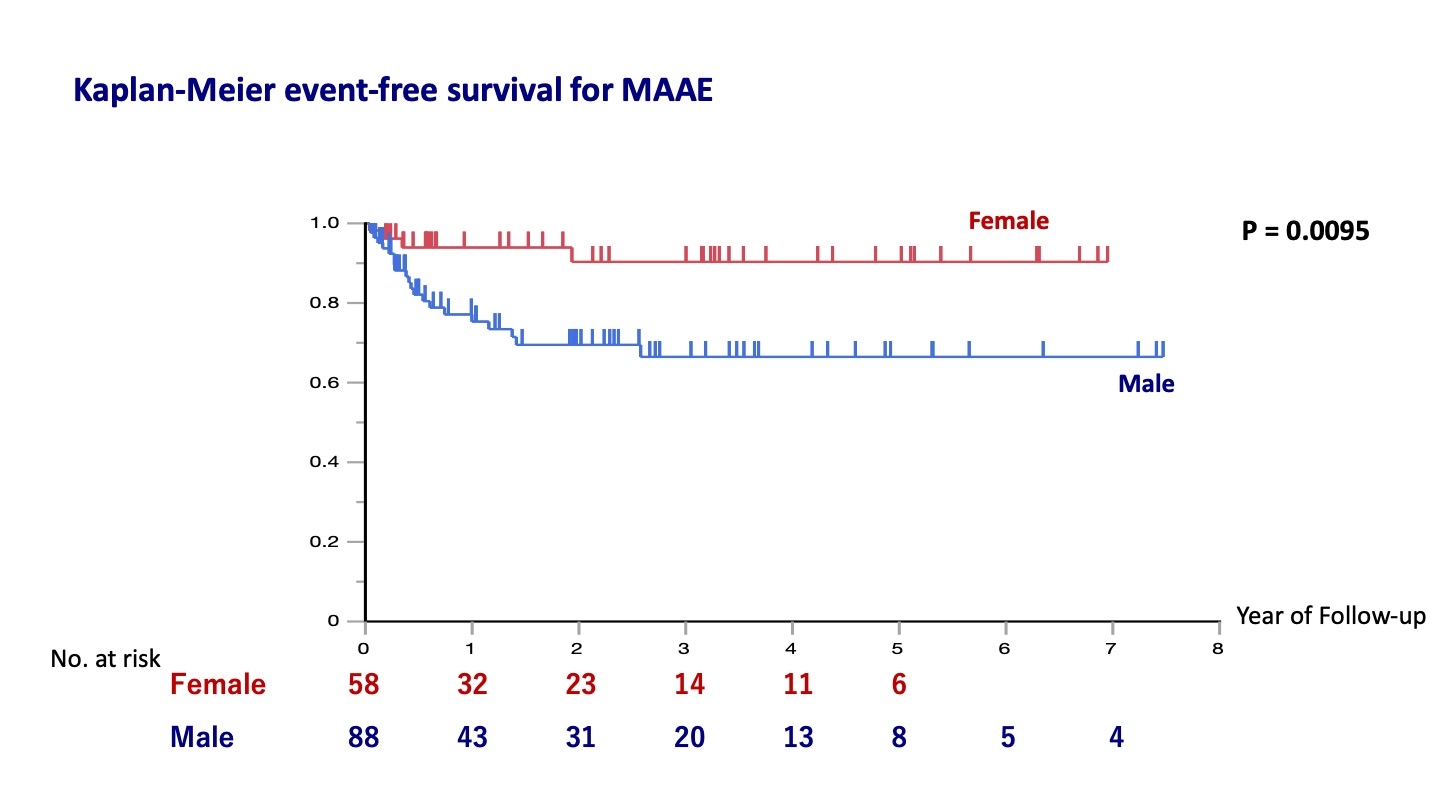
Results: Females were significantly older than male patients (73.0 vs 63.1 years; P<.0001). Females had lower body mass index (21.6 vs 23.2 kg/m2, p=0.016), lower geriatric nutritional risk index (93.2 vs 99.1; p=0.0017) and had less often a smoking habit (33% vs. 61%, p=0.00065) compared with males. More females presented with DeBakey class II as compared with males (33% vs. 61%, p<0.0001). Organ malperfusion was detected less frequently in females (17% vs 48% p=0.00011). While more complex procedures were chosen in males, operation time and cardiopulmonary time were not significantly different among males and females. Averaged follow-up time was 3.3 years and survival did not differ between genders. During follow-up, major adverse aortic events significantly occurred in men (log-rank P = 0.0095).
Conclusions: Women develop aortic dissection later in life. Despite women and men presenting at different ages and exhibiting varying dissection and malperfusion patterns, outcomes are similar in both genders. No differences were observed in both early and long-term mortality between females and males. Male patients had a significantly higher rate of major adverse aortic events. These results suggest that the decision-making for surgical treatment should not depend on gender, but that accounting for sex-specific risk factors rather than common risk factors may help to improve the outcome in both genders.
Methods: From September 2015 to December 2023, 146 patients, consisting of 58 women and 88 men, underwent surgery for acute type A aortic dissection at our institution. We compared clinical features and events between the 2 cohorts.
Results: Females were significantly older than male patients (73.0 vs 63.1 years; P<.0001). Females had lower body mass index (21.6 vs 23.2 kg/m2, p=0.016), lower geriatric nutritional risk index (93.2 vs 99.1; p=0.0017) and had less often a smoking habit (33% vs. 61%, p=0.00065) compared with males. More females presented with DeBakey class II as compared with males (33% vs. 61%, p<0.0001). Organ malperfusion was detected less frequently in females (17% vs 48% p=0.00011). While more complex procedures were chosen in males, operation time and cardiopulmonary time were not significantly different among males and females. Averaged follow-up time was 3.3 years and survival did not differ between genders. During follow-up, major adverse aortic events significantly occurred in men (log-rank P = 0.0095).
Conclusions: Women develop aortic dissection later in life. Despite women and men presenting at different ages and exhibiting varying dissection and malperfusion patterns, outcomes are similar in both genders. No differences were observed in both early and long-term mortality between females and males. Male patients had a significantly higher rate of major adverse aortic events. These results suggest that the decision-making for surgical treatment should not depend on gender, but that accounting for sex-specific risk factors rather than common risk factors may help to improve the outcome in both genders.
More abstracts on this topic:
A Hard Start: Early, Intensive Healthcare Utilization for Children with Critical Congenital Heart Disease
Ellis Danielle, Hall Matthew, Blume Elizabeth, Wolfe Joanne, Snaman Jennifer, Berry Jay
A Pressure-Volume Loops Approach Predicts Outcomes After Double Switch Operation For Congenitally Corrected Transposition Of The Great Arteries with Intact Ventricular SeptumThatte Nikhil, Del Nido Pedro, Ghelani Sunil, Hammer Peter, Marx Gerald, Beroukhim Rebecca, Gauvreau Kimberlee, Callahan Ryan, Prakash Ashwin, Emani Sitaram, Hoganson David