Final ID: MP1397
Timely diagnosed Giant Cell Myocarditis is not definitely lethal - A Rare Success Treatment
Abstract Body (Do not enter title and authors here): Giant cell myocarditis is a rare, rapidly progressive, potentially lethal disease caused by a T-cell-mediated inflammation of the myocardium. Rapid, early diagnosis is complicated by the diverse clinical picture (acute coronary syndrome, heart failure, arrhythmia episodes).
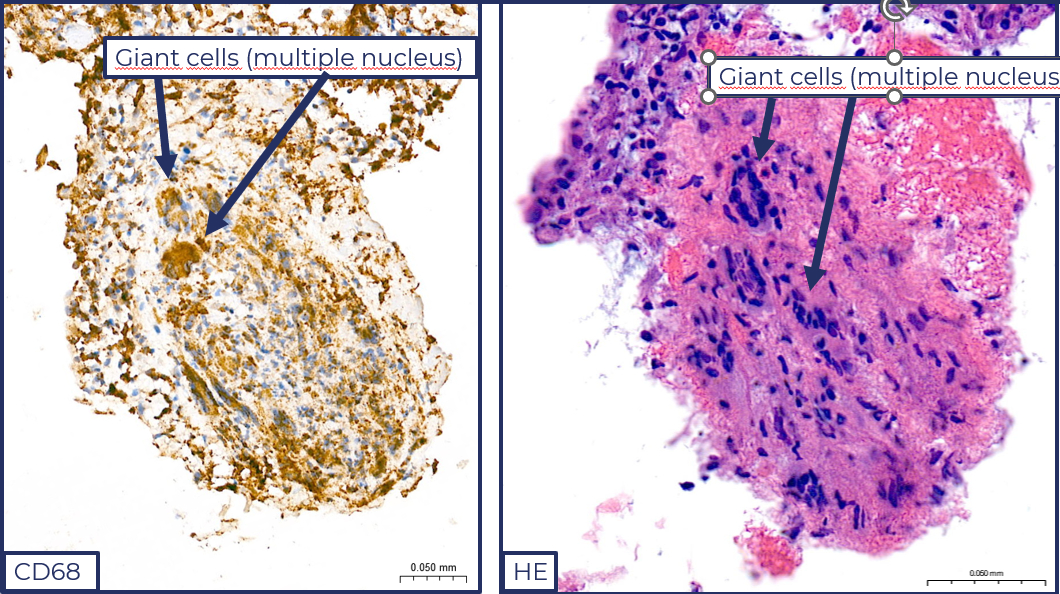
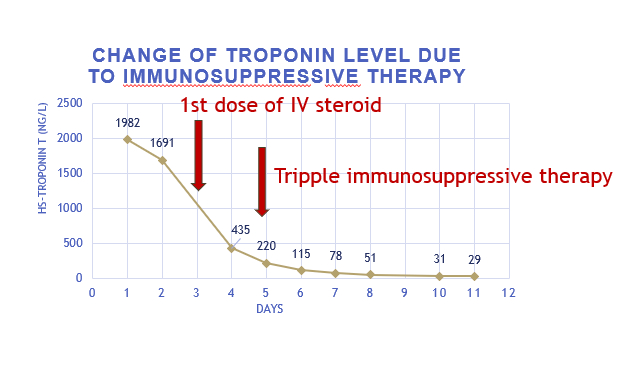
Our 52-year-old female patient has no significant medical history; she had an upper respiratory tract infection prior to admission. She presented to the ER with chest pain and dyspnea. ECG showed anterior ST-elevation. Urgent coronary angiography showed an intact coronary system. Initially, she was hemodynamically stable, and echocardiography showed a mildly reduced EF. During a short observation period, her condition rapidly progressed, she became hypotonic, and due to third-degree AV block and significant pausa, temporary PM implantation was performed. She was admitted to our clinic due to suspected progressive myocarditis. Her condition stabilized with dual circulatory support. Due to continuous PM requirement, performing cardiac MRI was not possible. Cardiac biopsy confirmed giant cell myocarditis. We started high-dose IV steroid therapy. As a result, left ventricular function improved and necroenzyme levels decreased. According to the latest literature recommendations, her steroid treatment was supplemented with mycophenolate mofetil and tacrolimus, which gradually improved the EF and AV conduction, eliminated the need for a pacemaker, we removed the iPM, and stopped the inotropes and vasopressors. Extensive bacteriological, viral serological and immunological tests did not confirm active infection or immunological abnormalities. Cardiac MRI showed good left and right ventricular ejection fractions and late non-ischemic contrast enhancement. She was discharged after 2 weeks of treatment in a stable clinical condition, with the use of complex immunosuppressive therapy. She receives regular follow-up in the heart transplantation department of our clinic. With immunosuppressive treatment, she is symptom-free, EF 60%, and has no arrhythmia or conduction disorders.
Our patient's case draws attention to the fact that in case of suspected myocarditis, myocardial biopsy and rapid diagnosis can be life-saving. It is rare that with combined immunosuppressive therapy and regular follow-up over a period of 1 year, the patient remained symptom-free, had good cardiac function, and was able to avoid possible heart transplantation and implantation of a circulatory support device.
Our 52-year-old female patient has no significant medical history; she had an upper respiratory tract infection prior to admission. She presented to the ER with chest pain and dyspnea. ECG showed anterior ST-elevation. Urgent coronary angiography showed an intact coronary system. Initially, she was hemodynamically stable, and echocardiography showed a mildly reduced EF. During a short observation period, her condition rapidly progressed, she became hypotonic, and due to third-degree AV block and significant pausa, temporary PM implantation was performed. She was admitted to our clinic due to suspected progressive myocarditis. Her condition stabilized with dual circulatory support. Due to continuous PM requirement, performing cardiac MRI was not possible. Cardiac biopsy confirmed giant cell myocarditis. We started high-dose IV steroid therapy. As a result, left ventricular function improved and necroenzyme levels decreased. According to the latest literature recommendations, her steroid treatment was supplemented with mycophenolate mofetil and tacrolimus, which gradually improved the EF and AV conduction, eliminated the need for a pacemaker, we removed the iPM, and stopped the inotropes and vasopressors. Extensive bacteriological, viral serological and immunological tests did not confirm active infection or immunological abnormalities. Cardiac MRI showed good left and right ventricular ejection fractions and late non-ischemic contrast enhancement. She was discharged after 2 weeks of treatment in a stable clinical condition, with the use of complex immunosuppressive therapy. She receives regular follow-up in the heart transplantation department of our clinic. With immunosuppressive treatment, she is symptom-free, EF 60%, and has no arrhythmia or conduction disorders.
Our patient's case draws attention to the fact that in case of suspected myocarditis, myocardial biopsy and rapid diagnosis can be life-saving. It is rare that with combined immunosuppressive therapy and regular follow-up over a period of 1 year, the patient remained symptom-free, had good cardiac function, and was able to avoid possible heart transplantation and implantation of a circulatory support device.
More abstracts on this topic:
Advanced Imaging for STEMI Mimicry: Diagnosing Myopericarditis in HIV
Bharaj Inderjeet Singh, Padda Inderbir, Brar Ajit, Mohmand Billal, Yeneneh Beeletsega, Sethi Yashendra
Cardiovascular Risk in Patients with Multiple Sclerosis: A 10-year Matched Cohort StudyAsjad Sayyed Jalawan, Zinabu Samrawit, Chhina Arashpreet, Chand Ali, Garlapati Sameer Krishna Prasad, Bowen Allan, Michael Miriam