Final ID: MP963
Comparison of Echocardiographic Pulmonary Artery Pressures to Pulmonary Artery Catheter Pulmonary Pressures in Patients on Peripheral VA-ECMO in an Academic Tertiary Care Hospital
Abstract Body (Do not enter title and authors here): Introduction
In patients requiring extracorporeal membrane oxygenation (ECMO), monitoring pulmonary artery systolic pressure (PASP) and assessing right ventricular (RV) function is crucial for guiding management. While transthoracic echocardiography offers noninvasive estimation of PASP (ePASP), its accuracy is not validated in ECMO patients. Direct pressure transduction is the gold standard for measuring true PASP (tPASP); however, its use carries risks, including infection, thrombosis, and mechanical complications. Given the invasive nature of PAC placement, an accurate noninvasive alternative could significantly reduce patient morbidity.
Methods
This is a retrospective observational study of patients who underwent peripheral VA-ECMO and received an echocardiogram, at MedStar Washington Hospital Center, between 1 January 2014 to 31 December 2024. Patients were included if they had an echocardiogram estimated PASP measurement within 1 hour of a directly transduced pressure measurement while on peripheral VA-ECMO. Exclusion criteria included patients on central VA-ECMO or VV-ECMO, insufficient TR jet to calculate PASP and patients with measurements more than 1 hour apart. Outcomes were modeled with R for statistical computing, using a spearman’s rank correlation, a mixed linear model.
Results
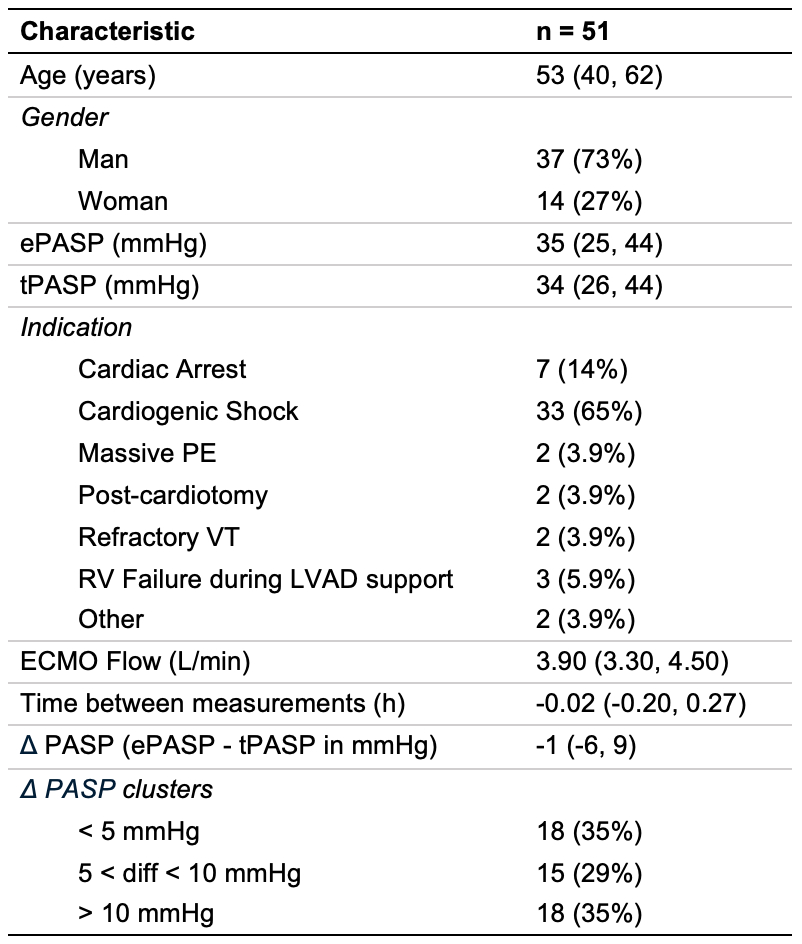
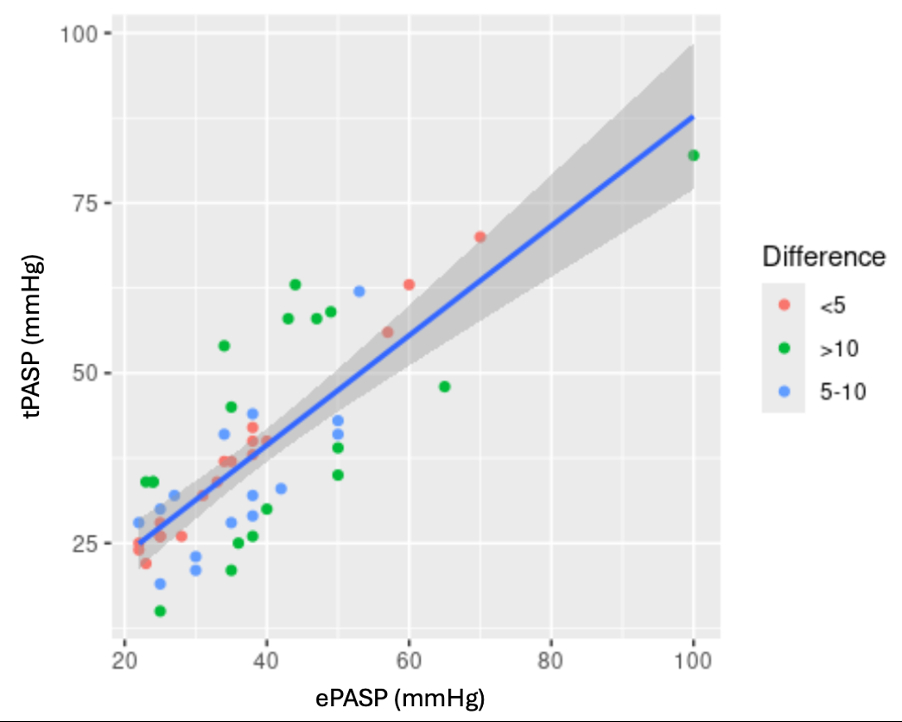
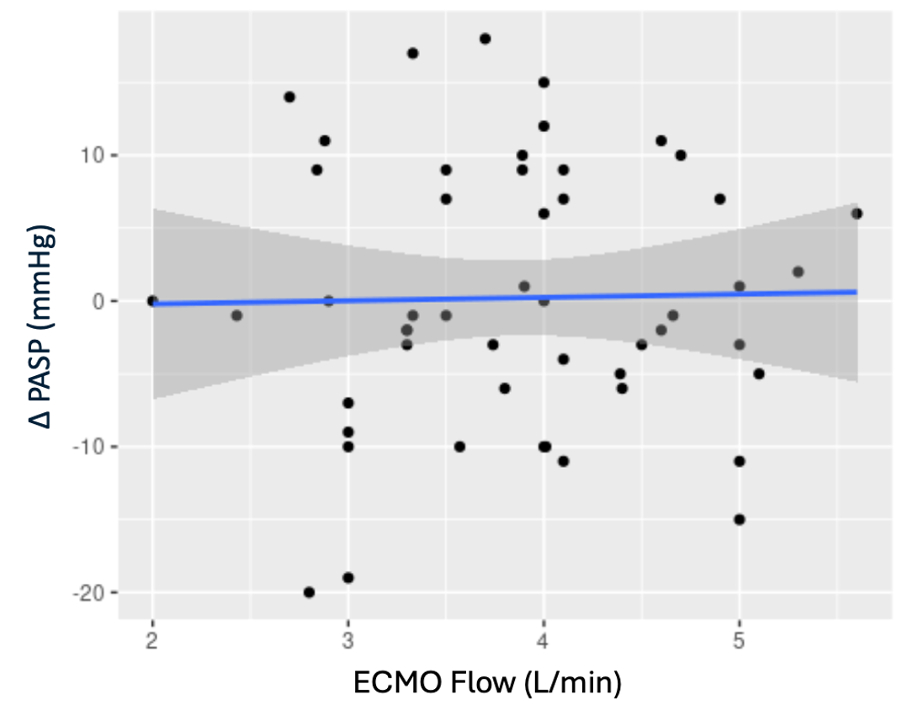
51 patients met study inclusion criteria. From the spearman’s rank correlation model, there was a strong positive correlation between ePASP and tPASP (ρ=0.73, p<0.001). In a linear mixed-effects model, ePASP was significantly associated with tPASP (β=0.81, 95% CI:0.64-0.98, p<0.001), with a marginal R2=0.647 and conditional R2=0.998. There was no correlation between the ECMO flow rate and ΔPASP, defined as ePASP - tPASP.
Discussion
This retrospective observational study demonstrates a positive correlation between ePASP and tPASP in patients on VA-ECMO. The model demonstrated excellent fit, with R2 values suggesting that both fixed and random effects accounted for nearly all observed variability. Our data suggest echocardiographic estimation of PASP remains accurate irrespective of ECMO flow rate. Future research is warranted to support broader adoption of echocardiography for hemodynamic assessment in VA-ECMO patients. Validating the reliability of echocardiographic estimates could support broader adoption of echocardiography for hemodynamic assessment in ECMO patients, minimizing the need for invasive monitoring and its associated risks.
In patients requiring extracorporeal membrane oxygenation (ECMO), monitoring pulmonary artery systolic pressure (PASP) and assessing right ventricular (RV) function is crucial for guiding management. While transthoracic echocardiography offers noninvasive estimation of PASP (ePASP), its accuracy is not validated in ECMO patients. Direct pressure transduction is the gold standard for measuring true PASP (tPASP); however, its use carries risks, including infection, thrombosis, and mechanical complications. Given the invasive nature of PAC placement, an accurate noninvasive alternative could significantly reduce patient morbidity.
Methods
This is a retrospective observational study of patients who underwent peripheral VA-ECMO and received an echocardiogram, at MedStar Washington Hospital Center, between 1 January 2014 to 31 December 2024. Patients were included if they had an echocardiogram estimated PASP measurement within 1 hour of a directly transduced pressure measurement while on peripheral VA-ECMO. Exclusion criteria included patients on central VA-ECMO or VV-ECMO, insufficient TR jet to calculate PASP and patients with measurements more than 1 hour apart. Outcomes were modeled with R for statistical computing, using a spearman’s rank correlation, a mixed linear model.
Results
51 patients met study inclusion criteria. From the spearman’s rank correlation model, there was a strong positive correlation between ePASP and tPASP (ρ=0.73, p<0.001). In a linear mixed-effects model, ePASP was significantly associated with tPASP (β=0.81, 95% CI:0.64-0.98, p<0.001), with a marginal R2=0.647 and conditional R2=0.998. There was no correlation between the ECMO flow rate and ΔPASP, defined as ePASP - tPASP.
Discussion
This retrospective observational study demonstrates a positive correlation between ePASP and tPASP in patients on VA-ECMO. The model demonstrated excellent fit, with R2 values suggesting that both fixed and random effects accounted for nearly all observed variability. Our data suggest echocardiographic estimation of PASP remains accurate irrespective of ECMO flow rate. Future research is warranted to support broader adoption of echocardiography for hemodynamic assessment in VA-ECMO patients. Validating the reliability of echocardiographic estimates could support broader adoption of echocardiography for hemodynamic assessment in ECMO patients, minimizing the need for invasive monitoring and its associated risks.
More abstracts on this topic:
2 Dimensional Echocardiography versus 3 Dimentional Echocardiography to Assess Right Ventricular Function in Pulmonary Hypertension: A Systematic Review
Chaudhry Waleed Razzaq, Hajj Fatima, Bathula Satyamedha, Meghji Mohammed Askari, Pasupuleti Hemalatha, Kiyani Madiha, Shah Syeda Simrah, Neelakantan Ramaswamy Sanathanan, Mirzaeidizaji Nakisa, St. Jacques Jahnoy, Khan Khalil Ullah, Veluchamy Elakkiya, Jesse Joshanna
2 Dimensional Echocardiography versus 3 Dimentional Echocardiography to Assess Right Ventricular Function in Pulmonary Hypertension: A Systematic ReviewChaudhry Waleed Razzaq, Hajj Fatima, Bathula Satyamedha, Meghji Mohammed Askari, Pasupuleti Hemalatha, Kiyani Madiha, Shah Syeda Simrah, Neelakantan Ramaswamy Sanathanan, Mirzaeidizaji Nakisa, St. Jacques Jahnoy, Khan Khalil Ullah, Veluchamy Elakkiya, Jesse Joshanna