Final ID: Mo3091
Tamponade and Reversible Cardiogenic Shock Due to Cyclophosphamide Myopericarditis After Haploidentical Stem Cell Transplant
Abstract Body (Do not enter title and authors here): Case
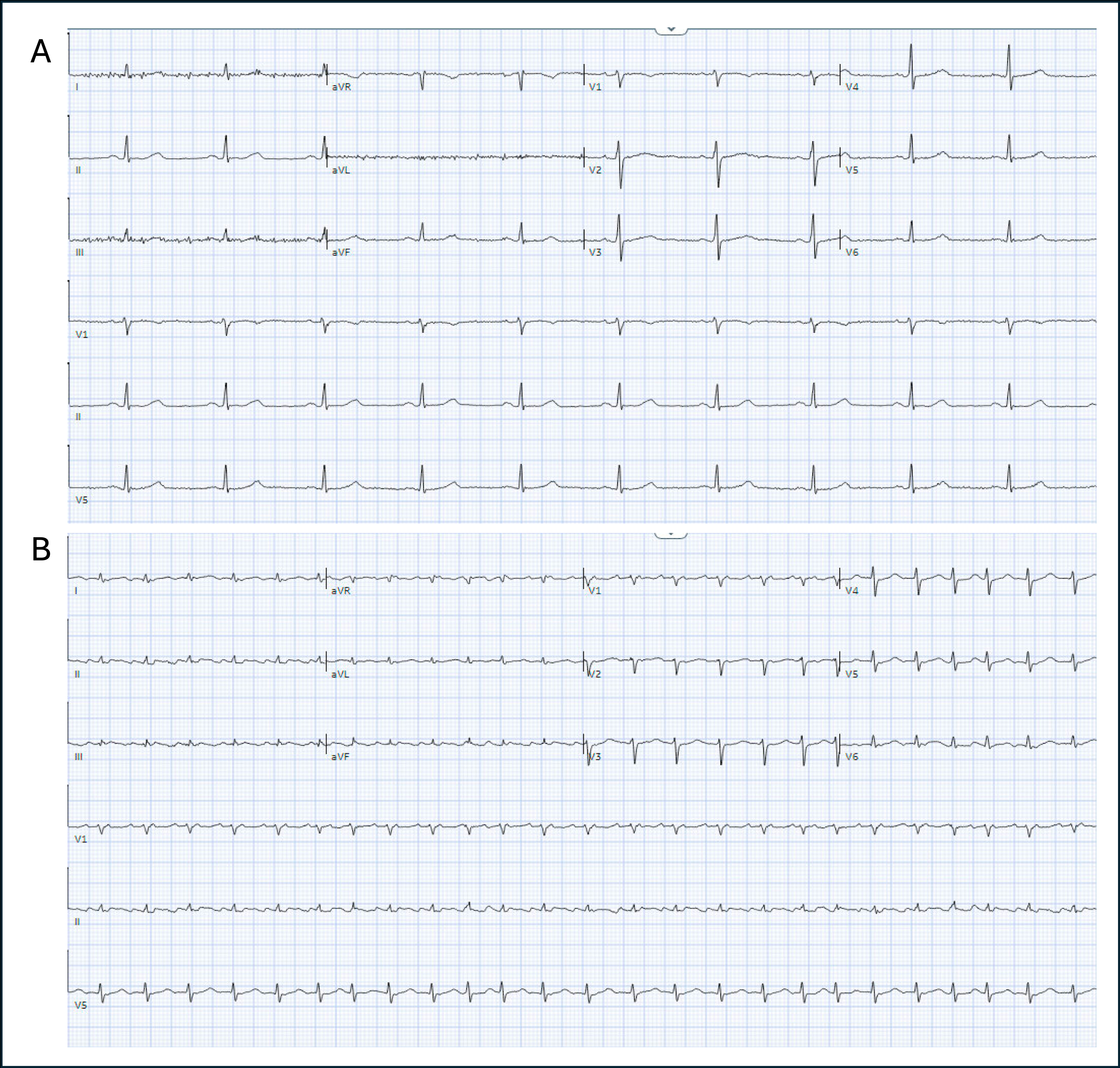
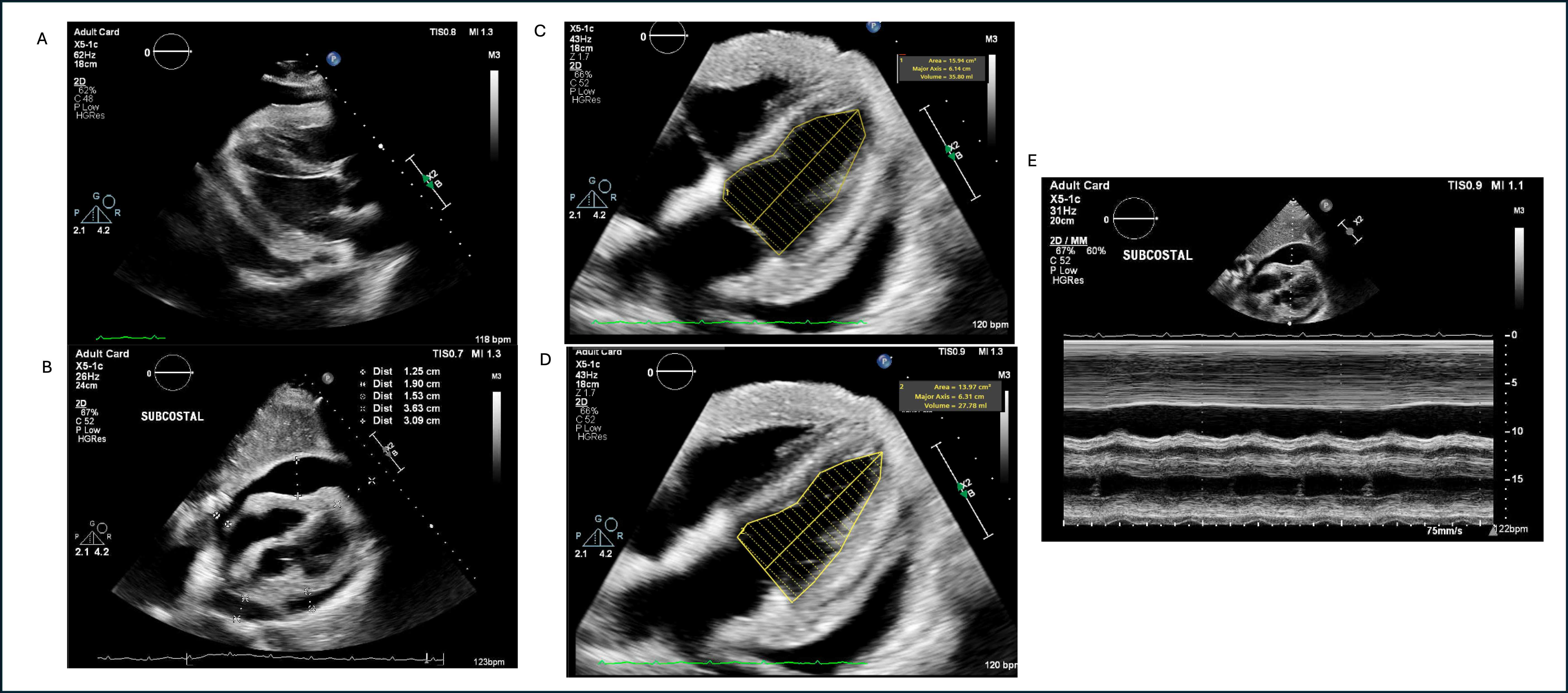
A 63-year-old man with history of Stage 4 Diffuse Large B-Cell Lymphoma and treatment-induced acute myeloid leukemia with incomplete hematologic recovery was admitted for reduced intensity conditioning with fludarabine followed by haplo stem cell transplantation. His prior cancer therapy included rituximab, cyclophosphamide, doxorubicin, vincristine, azacitidine, and venetoclax. He received post-transplant graft-versus-host prophylaxis with cyclophosphamide (PTCy) 50 mg/kg/day on days +3 and +4. On day +8, he became acutely hypotensive with blood pressure 81/61, tachycardic to 152 beats/min, and hypoxic to 86%. Physical exam revealed muffled heart sounds and jugular venous distention. An electrocardiogram showed new atrial flutter and decreased QRS voltage. Labs were notable for BNP 1,118 pg/mL and hs-troponin of 50 ng/L. He was started on norepinephrine and intubated for respiratory distress. Transthoracic echocardiogram (TTE) showed a large pericardial effusion with tamponade, reduction in LVEF from 50-55% to 20-25% and increased biventricular wall thickness. He underwent pericardiocentesis with removal of 700 mL of serous fluid. He was cross titrated to dobutamine for cardiogenic shock, which resolved within days. Cardiac MRI (CMR) on day +26 showed severe diffuse myocardial edema, diffuse midmyocardial late gadolinium enhancement, and pericardial enhancement. In this clinical setting, this was felt to be consistent with fulminant cyclophosphamide myopericarditis (Cy-MP). Subsequent TTE showed recovery of LVEF. He later developed aspiration, bacteremia, and graft failure and expired from septic shock.
Discussion:
Fulminant Cy-MP is thought to be highly fatal and is characterized by serosanguinous pericardial fluid, myocardial necrosis and fibrin microthrombi on autopsy. Unique findings in our case include serous pericardial fluid, only mild troponin rise, and recovery of LV systolic function, suggesting a more favorable presentation of Cy-MP. We also highlight the utility of CMR in antemortem diagnosis, given the often prohitibive risks of endomyocardial biopsy with comorbid cytopenia. Studies assessing early cardiotoxicity from PTCy support that recovery is possible, but long-term mortality risk remains elevated. The treatment of Cy-MP is supportive, and use of mechanical support is limited by cytopenia and prognostic concerns. Further investigation into risk factors for fulminant presentations, early detection, and tailored treatment is needed.
A 63-year-old man with history of Stage 4 Diffuse Large B-Cell Lymphoma and treatment-induced acute myeloid leukemia with incomplete hematologic recovery was admitted for reduced intensity conditioning with fludarabine followed by haplo stem cell transplantation. His prior cancer therapy included rituximab, cyclophosphamide, doxorubicin, vincristine, azacitidine, and venetoclax. He received post-transplant graft-versus-host prophylaxis with cyclophosphamide (PTCy) 50 mg/kg/day on days +3 and +4. On day +8, he became acutely hypotensive with blood pressure 81/61, tachycardic to 152 beats/min, and hypoxic to 86%. Physical exam revealed muffled heart sounds and jugular venous distention. An electrocardiogram showed new atrial flutter and decreased QRS voltage. Labs were notable for BNP 1,118 pg/mL and hs-troponin of 50 ng/L. He was started on norepinephrine and intubated for respiratory distress. Transthoracic echocardiogram (TTE) showed a large pericardial effusion with tamponade, reduction in LVEF from 50-55% to 20-25% and increased biventricular wall thickness. He underwent pericardiocentesis with removal of 700 mL of serous fluid. He was cross titrated to dobutamine for cardiogenic shock, which resolved within days. Cardiac MRI (CMR) on day +26 showed severe diffuse myocardial edema, diffuse midmyocardial late gadolinium enhancement, and pericardial enhancement. In this clinical setting, this was felt to be consistent with fulminant cyclophosphamide myopericarditis (Cy-MP). Subsequent TTE showed recovery of LVEF. He later developed aspiration, bacteremia, and graft failure and expired from septic shock.
Discussion:
Fulminant Cy-MP is thought to be highly fatal and is characterized by serosanguinous pericardial fluid, myocardial necrosis and fibrin microthrombi on autopsy. Unique findings in our case include serous pericardial fluid, only mild troponin rise, and recovery of LV systolic function, suggesting a more favorable presentation of Cy-MP. We also highlight the utility of CMR in antemortem diagnosis, given the often prohitibive risks of endomyocardial biopsy with comorbid cytopenia. Studies assessing early cardiotoxicity from PTCy support that recovery is possible, but long-term mortality risk remains elevated. The treatment of Cy-MP is supportive, and use of mechanical support is limited by cytopenia and prognostic concerns. Further investigation into risk factors for fulminant presentations, early detection, and tailored treatment is needed.
More abstracts on this topic:
Advanced Imaging for STEMI Mimicry: Diagnosing Myopericarditis in HIV
Bharaj Inderjeet Singh, Padda Inderbir, Brar Ajit, Mohmand Billal, Yeneneh Beeletsega, Sethi Yashendra
A Report of 2000 Consecutive Patients Undergoing Imaging with Pacemakers and ICDs in the MRI Environment; the Additive Value of a Large, Prospective ~20-Year Observational StudyBiederman Robert, Shah Moneal, Boltralik Mark, Williams Ronald, Lombardi Richard, Mangini Francesco, Doyle Mark