Final ID: MP1395
Equal Pressures, Unequal Outcomes: Diagnosing Constrictive Pericarditis in a Preserved Ejection Fraction Setting
Abstract Body (Do not enter title and authors here): Introduction:
Constrictive pericarditis (CP) is a rare but reversible cause of diastolic heart failure caused by chronic pericardial inflammation, fibrosis, and calcification that impairs ventricular filling. Often misdiagnosed as HFpEF (heart failure with preserved ejection fraction), CP has an estimated U.S. prevalence of 9–10 cases per million. Early recognition is crucial, as surgical pericardiectomy can be curative.
Case Presentation:
A 60-year-old male with hypertension, type 2 diabetes, and obstructive sleep apnea presented with progressive exertional dyspnea, fatigue, bilateral lower extremity edema, intermittent exertional chest pain, orthostatic dizziness, and palpitations.
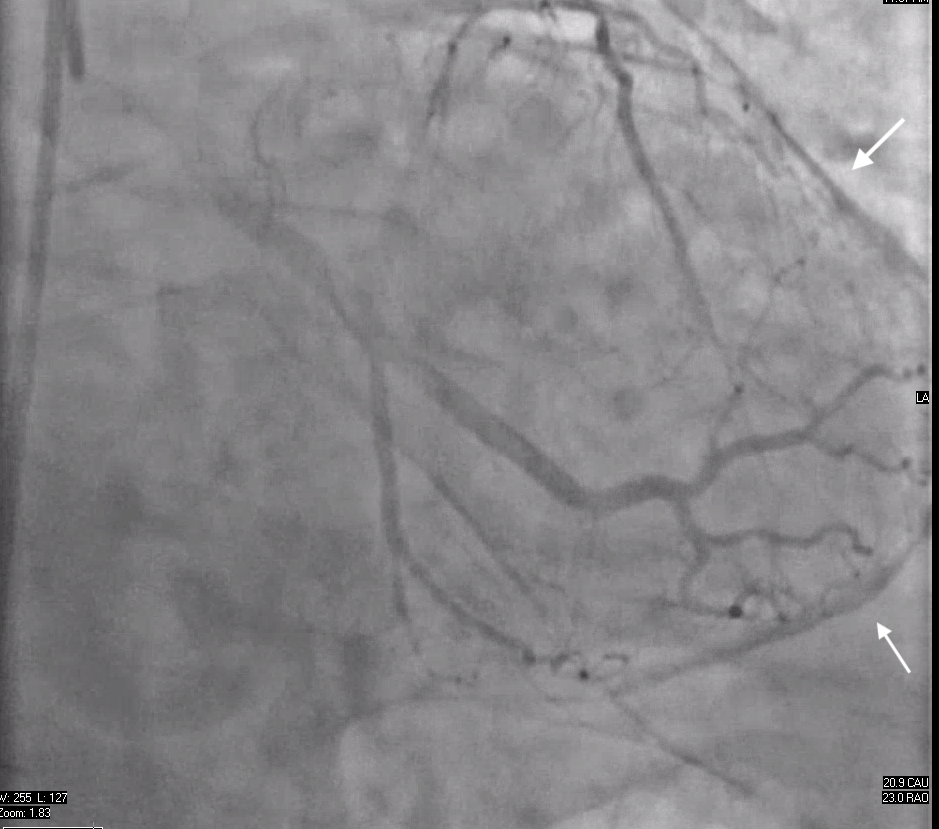
Initial evaluation in 2022 showed preserved left ventricular ejection fraction and no pericardial abnormalities on transthoracic echocardiogram. Myocardial perfusion SPECT revealed a mild right coronary artery perfusion defect. EKG showed right bundle branch block with nonspecific ST-T changes. In February 2024, left heart catheterization revealed mild coronary artery disease and incidental pericardial calcifications. By June 2024, CT angiography confirmed diffuse pericardial thickening and dense calcifications around the left ventricular apex, consistent with prior pericarditis.
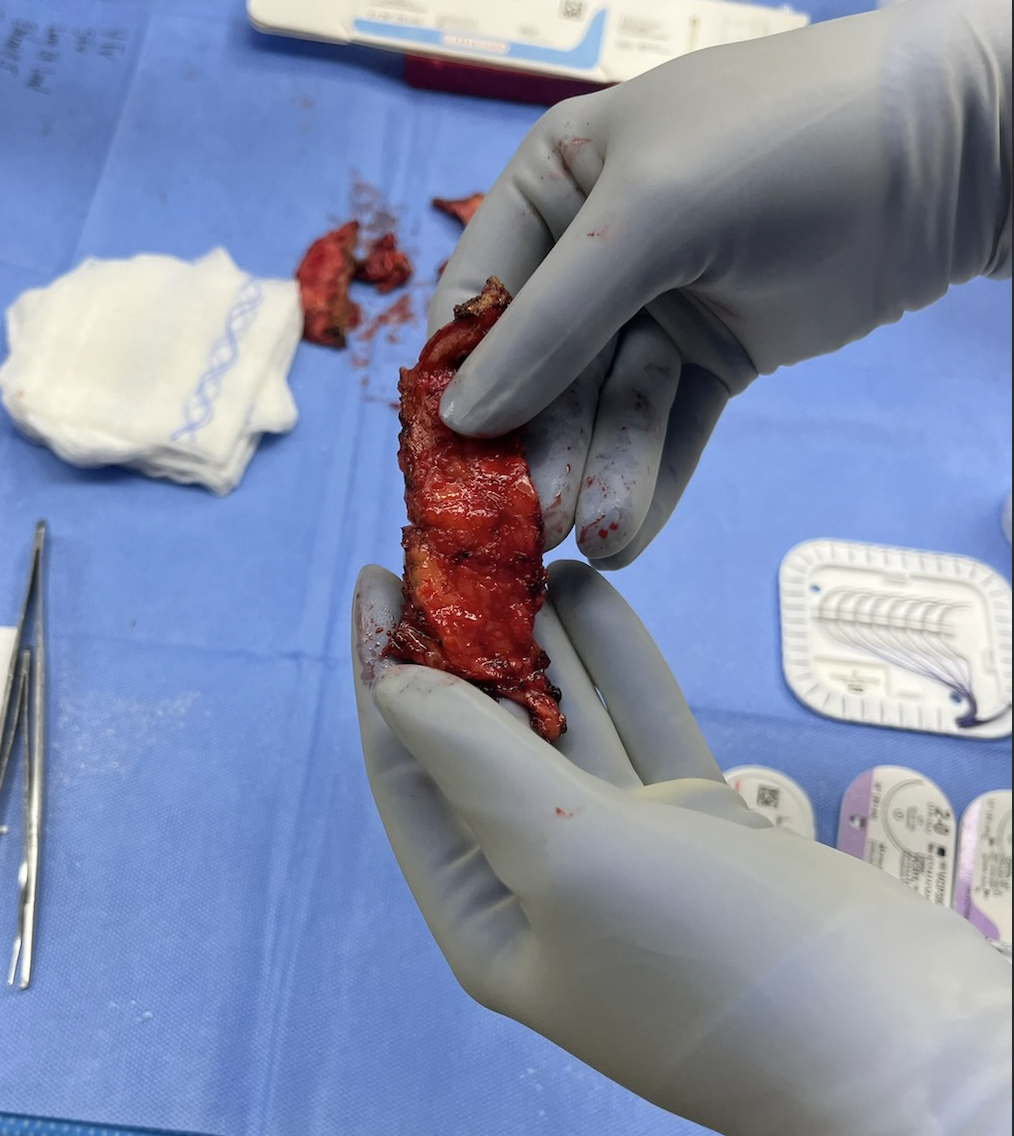
Right heart catheterization in July 2024 demonstrated equalization of diastolic pressures (Right Atrium: 25 mmHg, Right Ventricular End Diastolic Pressure: 24 mmHg, Pulmonary Capillary Wedge Pressure: 24 mmHg, Left Ventricular End Diastolic Pressure: 24–25 mmHg), reduced cardiac output (1.6 L/min), low cardiac index (1.7 L/min/m2), and mildly elevated Pulmonary Vascular Resistance (3.2 Wood units), confirming CP. The patient underwent pericardiectomy without cardiopulmonary bypass in August 2024. Pathology showed pericardial calcifications and chronic inflammation. Postoperatively, the patient reported improved exercise tolerance and resolution of symptoms.
Discussion:
This case highlights the diagnostic challenge of CP, especially in patients without classic risk factors such as prior surgery, radiation, or tuberculosis. The clinical picture mimicked HFpEF, but subtle clues—pericardial calcification and invasive hemodynamic findings—were critical for diagnosis. Timely pericardiectomy led to significant clinical improvement, emphasizing the importance of early recognition and intervention in CP.
Constrictive pericarditis (CP) is a rare but reversible cause of diastolic heart failure caused by chronic pericardial inflammation, fibrosis, and calcification that impairs ventricular filling. Often misdiagnosed as HFpEF (heart failure with preserved ejection fraction), CP has an estimated U.S. prevalence of 9–10 cases per million. Early recognition is crucial, as surgical pericardiectomy can be curative.
Case Presentation:
A 60-year-old male with hypertension, type 2 diabetes, and obstructive sleep apnea presented with progressive exertional dyspnea, fatigue, bilateral lower extremity edema, intermittent exertional chest pain, orthostatic dizziness, and palpitations.
Initial evaluation in 2022 showed preserved left ventricular ejection fraction and no pericardial abnormalities on transthoracic echocardiogram. Myocardial perfusion SPECT revealed a mild right coronary artery perfusion defect. EKG showed right bundle branch block with nonspecific ST-T changes. In February 2024, left heart catheterization revealed mild coronary artery disease and incidental pericardial calcifications. By June 2024, CT angiography confirmed diffuse pericardial thickening and dense calcifications around the left ventricular apex, consistent with prior pericarditis.
Right heart catheterization in July 2024 demonstrated equalization of diastolic pressures (Right Atrium: 25 mmHg, Right Ventricular End Diastolic Pressure: 24 mmHg, Pulmonary Capillary Wedge Pressure: 24 mmHg, Left Ventricular End Diastolic Pressure: 24–25 mmHg), reduced cardiac output (1.6 L/min), low cardiac index (1.7 L/min/m2), and mildly elevated Pulmonary Vascular Resistance (3.2 Wood units), confirming CP. The patient underwent pericardiectomy without cardiopulmonary bypass in August 2024. Pathology showed pericardial calcifications and chronic inflammation. Postoperatively, the patient reported improved exercise tolerance and resolution of symptoms.
Discussion:
This case highlights the diagnostic challenge of CP, especially in patients without classic risk factors such as prior surgery, radiation, or tuberculosis. The clinical picture mimicked HFpEF, but subtle clues—pericardial calcification and invasive hemodynamic findings—were critical for diagnosis. Timely pericardiectomy led to significant clinical improvement, emphasizing the importance of early recognition and intervention in CP.
More abstracts on this topic:
Anatomic Physiological Scoring is a Comparable Predictor of Adult Congenital Operative Morbidity and Mortality
La Brenda, Taylor-fishwick Jon, Macbeth Morgan, Soohoo Megan
Anomalous Origin Of Left Circumflex Artery From Right Pulmonary Artery Resulting In Heart Failure: A Rare Vascular Steal PhenomenonChander Yogesh, Bhardwaj Rajeev, Nandal Rajesh, Mittal Saurav, Pruthi Taniya, Singh Subeg