Final ID: MP895
Endovascular Intervention vs Surgical Bypass in Aorto-Iliac Disease
Abstract Body (Do not enter title and authors here): Background:
Aortoiliac disease, a subset of peripheral artery disease (PAD), frequently necessitates revascularization. While surgical bypass has long been the standard of care, endovascular intervention using stents is increasingly utilized. This study compared long-term outcomes in patients with aortoiliac PAD undergoing revascularization with endovascular intervention vs surgical bypasses.
Methods:
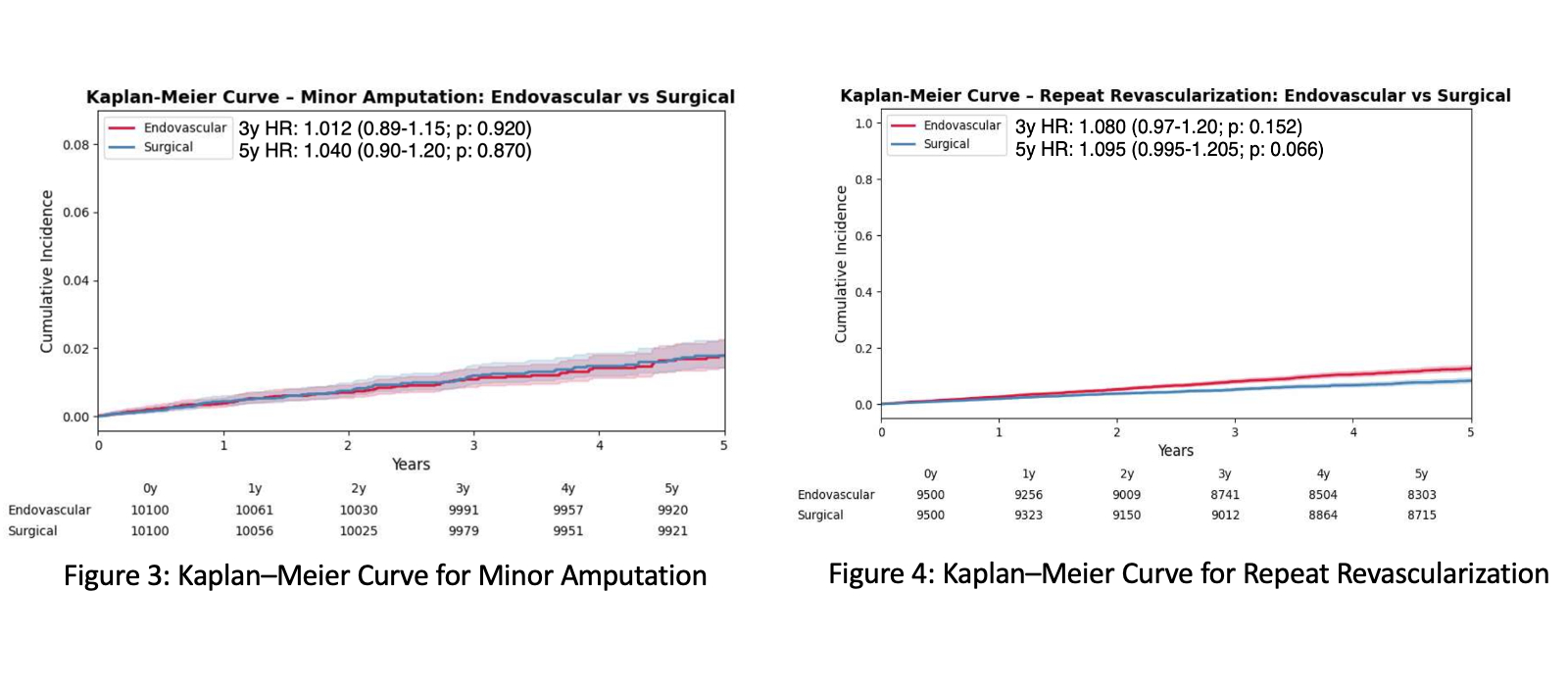
We conducted a retrospective cohort study using the TriNetX research network to identify patients with aortoiliac PAD who underwent lower extremity revascularization between January 1, 2010, and December 31, 2020. Patients were stratified by intervention type (endovascular interventions vs. surgical bypass) and matched 1:1 using propensity scores. Outcomes in propensity score matched cohort was evaluated at 3 and 5 years including all-cause mortality, major and minor amputations, repeat revascularization and chronic limb-threatening ischemia (CLTI) analyzed using Kaplan–Meier estimates and Cox proportional hazards models.
Results:
Of 28,825 patients with PAD, 14,576 received endovascular intervention and 14,245 received surgical bypass. Endovascular intervention recipients were older (Mean: 67 vs 65 years; P= 0.001) and males (60.9% vs 60.7%; p<0.001) and had higher prevalence of hypertension (66.3% vs 64.5%;p=0.005), hyperlipidemia (56.6% vs 53.9%; p<0.001), and diabetes (37.6% vs 33.7%; p=0.007). After matching (N = 10,232 per group), baseline demographics and comorbidities were well balanced. No significant differences existed in all-cause mortality (HR 1.03;0.952-1.119; p = 0.457), major amputation(0.97;0.87-1.08;p=0.42) minor amputation(1.040;0.9-1.2; p=0.87), chronic limb threatening ischemia (HR 0.995;0.88–1.12; p=0.970) and repeat revascularization (HR 1.095;0.995-1.205, p = 0.066) between the endovascular intervention and surgical bypass cohorts. A male-specific sensitivity analysis showed no significant difference in survival (mean difference
+1.19%; 95% CI= −0.17% to +2.61%)
Conclusion:
Endovascular intervention and surgical bypass demonstrated comparable long-term outcomes in this large, real-world cohort. These findings support endovascular therapy as a viable alternative to surgical revascularization, even in anatomically complex aortoiliac lesions. Further randomized controlled trials are warranted to guide treatment strategies in this population.
Aortoiliac disease, a subset of peripheral artery disease (PAD), frequently necessitates revascularization. While surgical bypass has long been the standard of care, endovascular intervention using stents is increasingly utilized. This study compared long-term outcomes in patients with aortoiliac PAD undergoing revascularization with endovascular intervention vs surgical bypasses.
Methods:
We conducted a retrospective cohort study using the TriNetX research network to identify patients with aortoiliac PAD who underwent lower extremity revascularization between January 1, 2010, and December 31, 2020. Patients were stratified by intervention type (endovascular interventions vs. surgical bypass) and matched 1:1 using propensity scores. Outcomes in propensity score matched cohort was evaluated at 3 and 5 years including all-cause mortality, major and minor amputations, repeat revascularization and chronic limb-threatening ischemia (CLTI) analyzed using Kaplan–Meier estimates and Cox proportional hazards models.
Results:
Of 28,825 patients with PAD, 14,576 received endovascular intervention and 14,245 received surgical bypass. Endovascular intervention recipients were older (Mean: 67 vs 65 years; P= 0.001) and males (60.9% vs 60.7%; p<0.001) and had higher prevalence of hypertension (66.3% vs 64.5%;p=0.005), hyperlipidemia (56.6% vs 53.9%; p<0.001), and diabetes (37.6% vs 33.7%; p=0.007). After matching (N = 10,232 per group), baseline demographics and comorbidities were well balanced. No significant differences existed in all-cause mortality (HR 1.03;0.952-1.119; p = 0.457), major amputation(0.97;0.87-1.08;p=0.42) minor amputation(1.040;0.9-1.2; p=0.87), chronic limb threatening ischemia (HR 0.995;0.88–1.12; p=0.970) and repeat revascularization (HR 1.095;0.995-1.205, p = 0.066) between the endovascular intervention and surgical bypass cohorts. A male-specific sensitivity analysis showed no significant difference in survival (mean difference
+1.19%; 95% CI= −0.17% to +2.61%)
Conclusion:
Endovascular intervention and surgical bypass demonstrated comparable long-term outcomes in this large, real-world cohort. These findings support endovascular therapy as a viable alternative to surgical revascularization, even in anatomically complex aortoiliac lesions. Further randomized controlled trials are warranted to guide treatment strategies in this population.
More abstracts on this topic:
Design of Extracranial-Intracranial Bypass Surgery for Symptomatic Chronic Middle Cerebral Artery Occlusion Trial (CMOSS-2)
Ma Yan, Wang Tao, Wang Haibo, Yang Yifan, Wang Jie, Derdeyn Colin, Gu Yuxiang, Jiao Liqun
Advanced Age Increases Susceptibility to Ischemic Myopathy after Murine Hindlimb IschemiaKulkarni Deepali, Massie Pierce, Justus Matthew, Mazloumibakhshayesh Milad, Coffman Brittany, Pace Carolyn, Clark Ross