Final ID: Sa3117
Outcomes of Non-Cardiac Surgery Following Transcatheter Mitral Valve Replacement: A US Collaborative Network Cohort Study
Abstract Body (Do not enter title and authors here): Introduction
Transcatheter mitral valve replacement (TMVR) offers a less invasive alternative to traditional open-heart surgery for patients with mitral valve disease. Despite its growing use, there has been limited research on the post-procedural stratification of patients undergoing TMVR, particularly in relation to non-cardiac surgery (NCS).
Methods
Data was retrospectively collected from the US-based TriNetX network, which includes 120 million patients across 70+ healthcare organizations. We identified patients aged ≥50 who underwent TMVR between 2014 and 2025, excluding those with concomitant aortic replacements. Patients were divided into two cohorts: those who underwent NCS and those who did not. A 1:1 propensity score matching (PSM) was performed based on demographics and comorbidities. Hazard ratios were used to assess overall survival (OS) and outcomes at 1 and 3 years.
Results
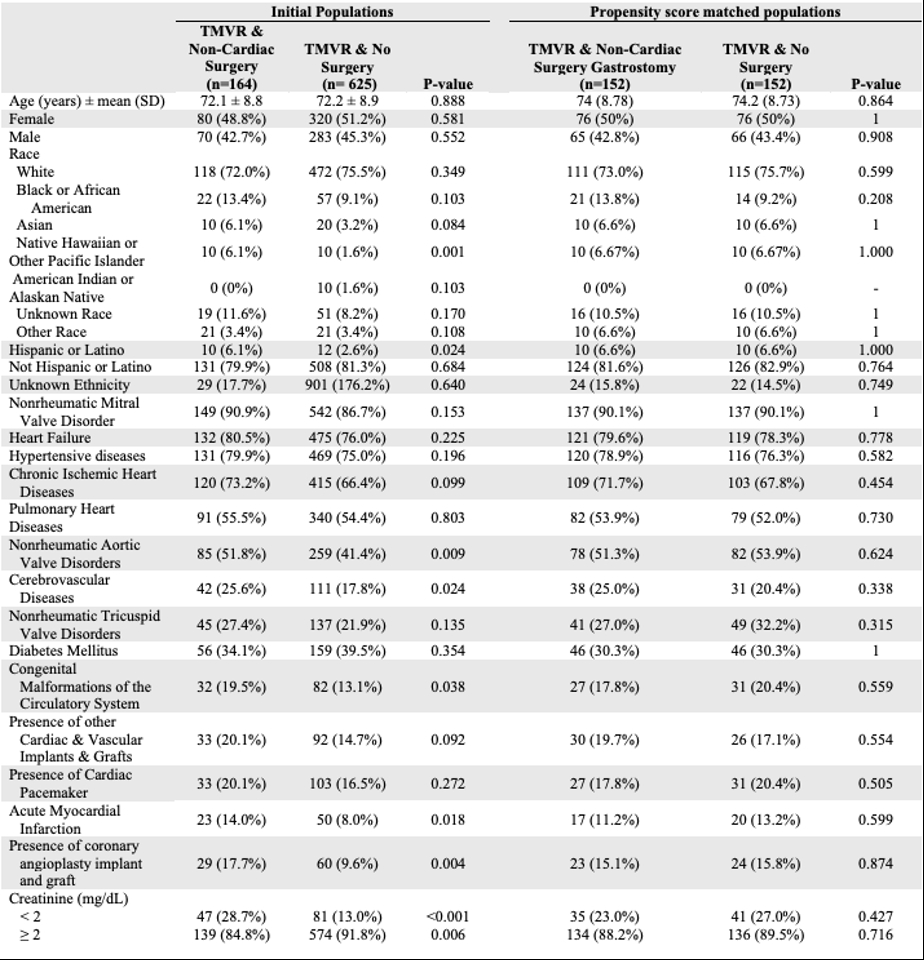
We identified 789 patients aged 50 and above who underwent TMVR exclusively. After matching, each cohort included 152 patients. Cohort characteristics before and after matching are presented in Table 1. The group that underwent NCS exhibited significantly worse OS at both 1 year (hazard ratio [HR], 2.40 [95% CI, 1.30-4.42]) and 3 years (HR, 2.21 [95% CI, 1.37-3.57]). Additionally, readmission rates were notably higher in the NCS at 1 year (HR, 2.96 [95% CI, 1.89-4.66]) and 3 years (HR, 2.71 [95% CI, 1.79-4.12]). Gastrointestinal bleeding was also significantly more frequent in the NCS cohort at both 1 year (HR, 7.74 [95% CI, 3.28-18.28]) and 3 years (HR, 4.98 [95% CI, 2.57- 9.64]). The risk of acute kidney injury (AKI) was elevated in the NCS group at 1 year (HR, 4.69 [95% CI, 2.61-8.46]) and 3 years (HR, 4.28 [95% CI, 2.56-7.15]). However, there were no significant differences between groups regarding stroke or new-onset atrial fibrillation.
Conclusion
Patients who underwent NCS following TMVR experienced significantly worse outcomes compared to those who did not. These patients had higher risks of mortality, readmission, gastrointestinal bleeding, and AKI at both 1- and 3-year post-procedure. Patients undergoing TMVR who undergo NCS appear to be a particularly high-risk group and may benefit from targeted therapies and meticulous postoperative care.
Transcatheter mitral valve replacement (TMVR) offers a less invasive alternative to traditional open-heart surgery for patients with mitral valve disease. Despite its growing use, there has been limited research on the post-procedural stratification of patients undergoing TMVR, particularly in relation to non-cardiac surgery (NCS).
Methods
Data was retrospectively collected from the US-based TriNetX network, which includes 120 million patients across 70+ healthcare organizations. We identified patients aged ≥50 who underwent TMVR between 2014 and 2025, excluding those with concomitant aortic replacements. Patients were divided into two cohorts: those who underwent NCS and those who did not. A 1:1 propensity score matching (PSM) was performed based on demographics and comorbidities. Hazard ratios were used to assess overall survival (OS) and outcomes at 1 and 3 years.
Results
We identified 789 patients aged 50 and above who underwent TMVR exclusively. After matching, each cohort included 152 patients. Cohort characteristics before and after matching are presented in Table 1. The group that underwent NCS exhibited significantly worse OS at both 1 year (hazard ratio [HR], 2.40 [95% CI, 1.30-4.42]) and 3 years (HR, 2.21 [95% CI, 1.37-3.57]). Additionally, readmission rates were notably higher in the NCS at 1 year (HR, 2.96 [95% CI, 1.89-4.66]) and 3 years (HR, 2.71 [95% CI, 1.79-4.12]). Gastrointestinal bleeding was also significantly more frequent in the NCS cohort at both 1 year (HR, 7.74 [95% CI, 3.28-18.28]) and 3 years (HR, 4.98 [95% CI, 2.57- 9.64]). The risk of acute kidney injury (AKI) was elevated in the NCS group at 1 year (HR, 4.69 [95% CI, 2.61-8.46]) and 3 years (HR, 4.28 [95% CI, 2.56-7.15]). However, there were no significant differences between groups regarding stroke or new-onset atrial fibrillation.
Conclusion
Patients who underwent NCS following TMVR experienced significantly worse outcomes compared to those who did not. These patients had higher risks of mortality, readmission, gastrointestinal bleeding, and AKI at both 1- and 3-year post-procedure. Patients undergoing TMVR who undergo NCS appear to be a particularly high-risk group and may benefit from targeted therapies and meticulous postoperative care.
More abstracts on this topic:
A Multimodality Education Model Improves Healthcare Professionals' Competency in Managing Cardiovascular Risk Factors in Type 2 Diabetes: A Mixed-Methods Study
Madhusudhan Divya, Pressley Alyssa, El Sayed Nuha, Okeke Oge, Bradley Sarah, Blanco Caroline, Perla Esteban, Jennings Ruby, Picou Kylie, Mcweeny Patrick, Crabill Carrianne
A Stepwise Approach to Identifying and Assessing the Content Validity of Patient-Reported Outcome (PRO) Measures for Use with Adults with Acute Heart FailureO'connor Meaghan, Loughlin Anita, Waldman Laura, Rucker Sloan, Vaghela Shailja, Kwon Namhee, Sikirica Vanja