Final ID: Su2092
Limited English Proficiency Is Linked to Gaps in Cardiovascular Follow-Up and Cardiac Comorbidity Capture
Abstract Body (Do not enter title and authors here): Introduction:
Cardiovascular disease (CVD) disproportionately affects South Asians, with Nepali-speaking limited English proficiency (N-LEP) community at particularly high risk. In Western Pennsylvania, N-LEP refugees are the fastest-growing LEP group, and despite elevated risk, CVD care patterns remain understudied. While acute care is driven by symptom severity, outpatient (OP) follow-up depends on health literacy, system navigation, and language access—areas where LEP patients face barriers, leading to underdiagnosis and long-term adverse outcomes.
Hypothesis:
N-LEP patients have lower OP follow-up after CV admissions than English-speaking patients (ES), contributing to underdiagnosis. Interpreter use and emergency care timeliness were also assessed.
Methods:
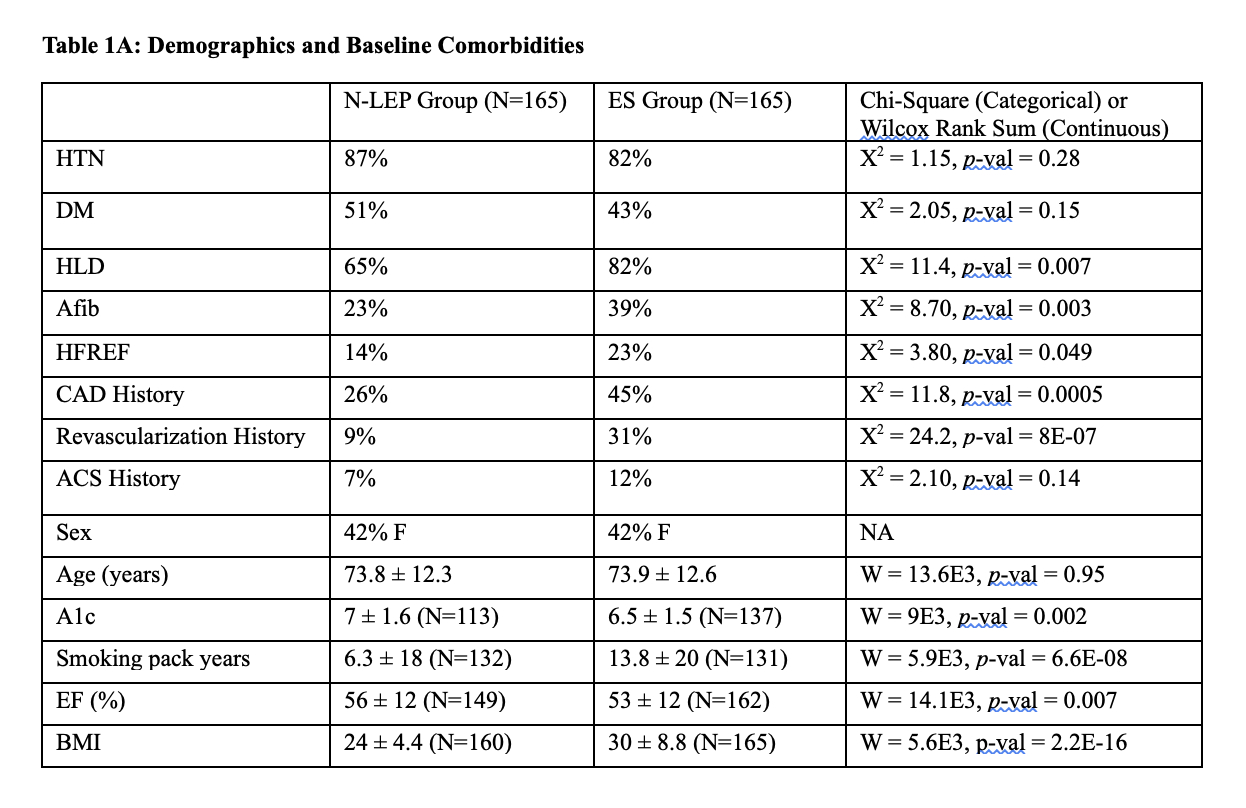
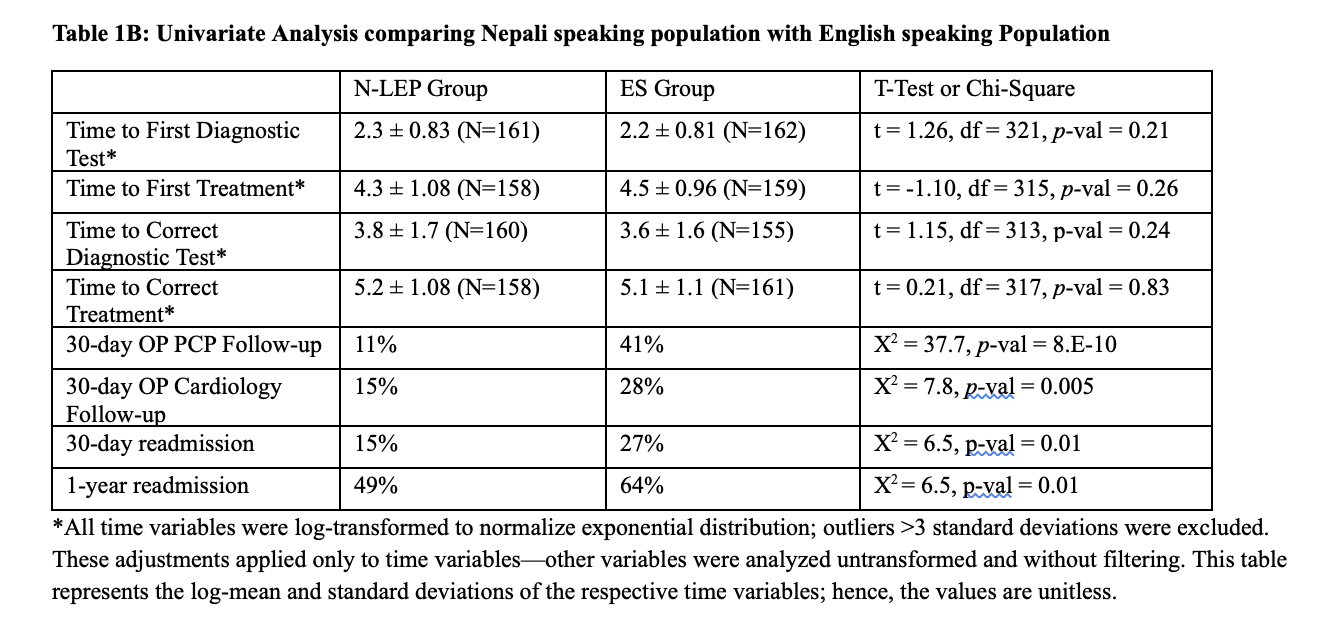
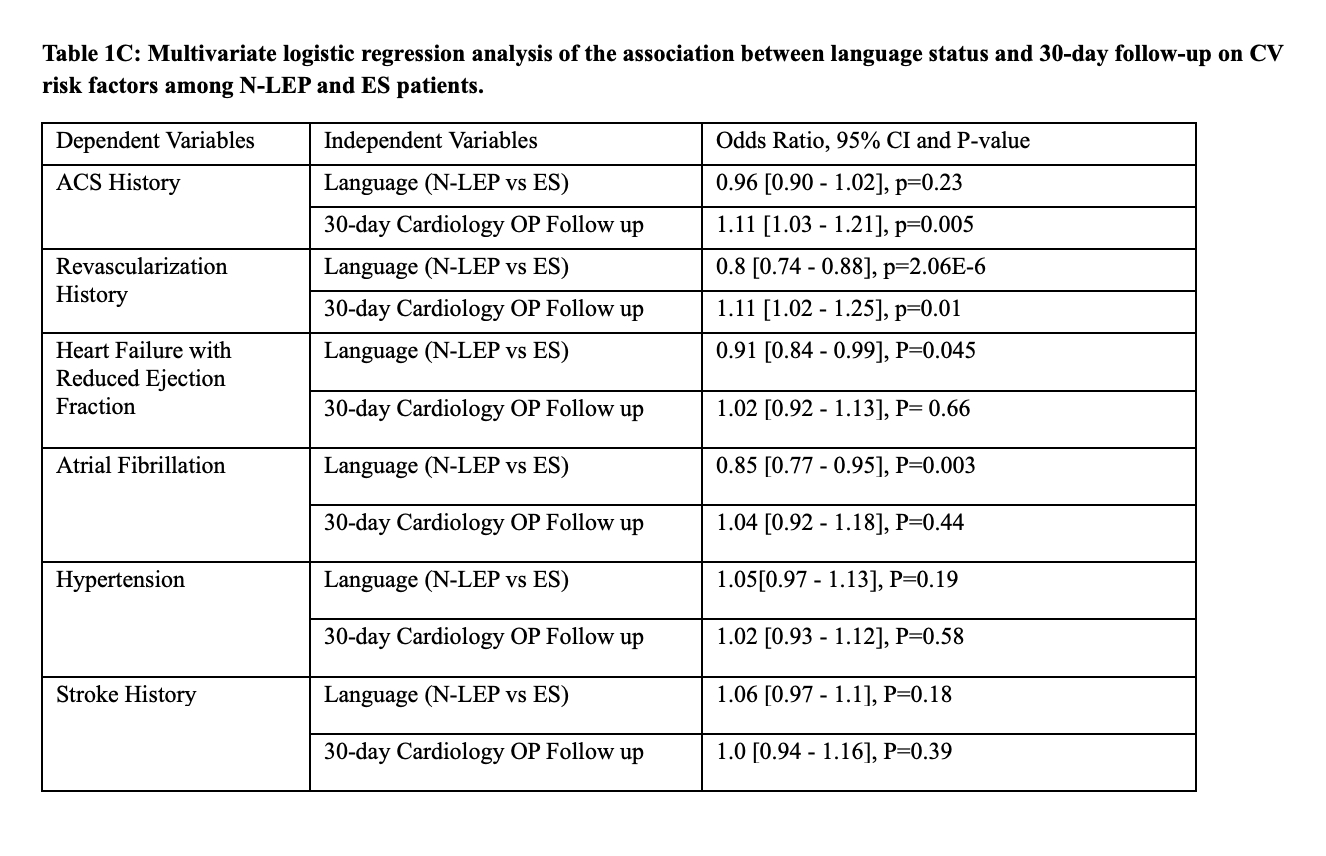
We retrospectively reviewed 165 N-LEP and 165 age-, gender-, and diagnosis-matched ES CV admissions at a Pittsburgh community hospital (2017–2024). Baseline CV comorbidities were collected. The primary outcome was 30-day follow-up (primary care or cardiology). Interpreter use (family, phone, or none), readmissions, and time to treatment were recorded. Time variables were log-transformed. Analyses included multivariable regression, Chi-square, and Wilcoxon rank-sum tests.
Results:
N-LEP patients had lower 30-day follow-up with primary care (10% vs 41%) and cardiology (15% vs 28%), and fewer 30-day (15% vs 27%) and 1-year (49% vs 64%) readmissions (p<0.05). Diagnostic (log mean: 3.9 vs 3.8) and treatment (5.3 vs 5.2) times were similar (p>0.3). ES patients had more comorbidities: HLD (81% vs 65%), ACS (13% vs 3%), and revascularization (31% vs 5%) (p<0.05). In multivariable analysis, ACS history was not predicted by language after adjusting for 30-day cardiology follow-up (OR 0.96, p=0.23), but follow-up was associated with higher ACS documentation (OR 1.1, p=0.005). Interpreters were used in 95% of N-LEP encounters; 88% involved family. Interpreter type did not affect care timelines.
Conclusion:
Despite similar acute care timelines, N-LEP patients had significantly lower OP follow-up. This was linked to fewer recorded comorbidities, likely due to missed chances for longitudinal assessment and CV risk mitigation. Our findings reflect gaps in continuity of care leading to under documentation rather than truly equitable outcomes. Interpreter use alone didnot mitigate disparities, suggesting structural, cultural & access barriers require broader solutions beyond translation to ensure equity in CV outcomes.
Cardiovascular disease (CVD) disproportionately affects South Asians, with Nepali-speaking limited English proficiency (N-LEP) community at particularly high risk. In Western Pennsylvania, N-LEP refugees are the fastest-growing LEP group, and despite elevated risk, CVD care patterns remain understudied. While acute care is driven by symptom severity, outpatient (OP) follow-up depends on health literacy, system navigation, and language access—areas where LEP patients face barriers, leading to underdiagnosis and long-term adverse outcomes.
Hypothesis:
N-LEP patients have lower OP follow-up after CV admissions than English-speaking patients (ES), contributing to underdiagnosis. Interpreter use and emergency care timeliness were also assessed.
Methods:
We retrospectively reviewed 165 N-LEP and 165 age-, gender-, and diagnosis-matched ES CV admissions at a Pittsburgh community hospital (2017–2024). Baseline CV comorbidities were collected. The primary outcome was 30-day follow-up (primary care or cardiology). Interpreter use (family, phone, or none), readmissions, and time to treatment were recorded. Time variables were log-transformed. Analyses included multivariable regression, Chi-square, and Wilcoxon rank-sum tests.
Results:
N-LEP patients had lower 30-day follow-up with primary care (10% vs 41%) and cardiology (15% vs 28%), and fewer 30-day (15% vs 27%) and 1-year (49% vs 64%) readmissions (p<0.05). Diagnostic (log mean: 3.9 vs 3.8) and treatment (5.3 vs 5.2) times were similar (p>0.3). ES patients had more comorbidities: HLD (81% vs 65%), ACS (13% vs 3%), and revascularization (31% vs 5%) (p<0.05). In multivariable analysis, ACS history was not predicted by language after adjusting for 30-day cardiology follow-up (OR 0.96, p=0.23), but follow-up was associated with higher ACS documentation (OR 1.1, p=0.005). Interpreters were used in 95% of N-LEP encounters; 88% involved family. Interpreter type did not affect care timelines.
Conclusion:
Despite similar acute care timelines, N-LEP patients had significantly lower OP follow-up. This was linked to fewer recorded comorbidities, likely due to missed chances for longitudinal assessment and CV risk mitigation. Our findings reflect gaps in continuity of care leading to under documentation rather than truly equitable outcomes. Interpreter use alone didnot mitigate disparities, suggesting structural, cultural & access barriers require broader solutions beyond translation to ensure equity in CV outcomes.
More abstracts on this topic:
All Magnesium-Based Bioresorbable Scaffolds in patients with CAD: A Proportional Meta Analysis
Dar Areej, Abu Ajamieh Kamal, Abdullah Muhammad, Khalid Ghina, Kamel Mohammed, Dar Muhammad Shayaan
2 Dimensional Echocardiography versus 3 Dimentional Echocardiography to Assess Right Ventricular Function in Pulmonary Hypertension: A Systematic ReviewChaudhry Waleed Razzaq, Hajj Fatima, Bathula Satyamedha, Meghji Mohammed Askari, Pasupuleti Hemalatha, Kiyani Madiha, Shah Syeda Simrah, Neelakantan Ramaswamy Sanathanan, Mirzaeidizaji Nakisa, St. Jacques Jahnoy, Khan Khalil Ullah, Veluchamy Elakkiya, Jesse Joshanna