Final ID: Su2029
Area-Based Social Risk Measures and In-Hospital Mortality: A Comparative Modeling Study in Coronary Artery Disease Patients
Abstract Body (Do not enter title and authors here):
Introduction
While risk prediction of cardiovascular outcomes, including in-hospital mortality, increasingly incorporates social determinants of health (SDOH), it remains unclear which area-level SDOH indices are most informative for predicting in-hospital mortality. Multiple area-level SDOH indices exist including the Social Vulnerability Index (SVI), Social Deprivation Index (SDI), Distressed Communities Index (DCI), Area Deprivation Index (ADI), Environmental Justice Index (EJI), Structural Racism Effect Index (SREI), and Community Deprivation Index (CDI).
Objective
The study aims to test the hypothesis that risk prediction of in-hospital mortality in patients with coronary artery disease may differ based on the specific SDOH index utilized.
Methods
We conducted a cohort study using data (2021-2023) from the Get with The Guidelines®–Coronary Artery Disease (GWTG-CAD) registry, linked to seven SDOH indices via patient’s residential ZIP code. For this linkage, Census tract-level SDOH indices were population-weighted to the ZIP code level. Correlations among indices were assessed using Pearson coefficients. To examine associations between each index and in-hospital mortality, generalized linear mixed models were used adjusting for potential confounders (e.g., age, sex, medical history and clinical presentation). Patients were categorized into quintiles using SDOH index (Q1 = least disadvantaged as reference, Q5 = most disadvantaged).
Results
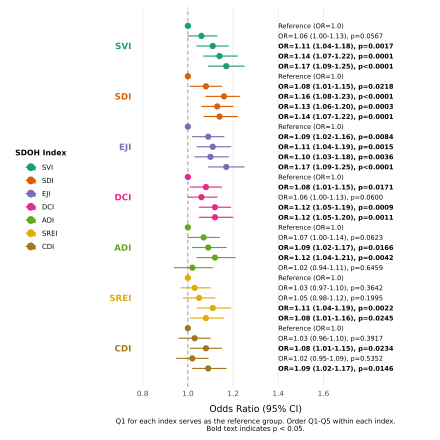
Among 283,586 patients (median age 65 [IQR 18]; 33.3% female; 70.4% non-Hispanic White; 13.7% Black), correlations among the indices varied (r = 0.41–0.83), with strong correlations observed between SVI–EJI (r = 0.81) and SVI–CDI (r = 0.83). ADI showed weaker correlations (e.g., ADI–SDI r = 0.41; ADI–SVI r = 0.47)., Higher quintiles (greater social disadvantage) were generally associated with increased in-hospital mortality; but the strength and consistency varied among seven indices (Figure 1). SVI showed a clear and steady increase in mortality risk across quintiles, while ADI, SREI, and CDI had inconsistent relationships with in-hospital mortality.
Conclusions
Not all SDOH indices are equally predictive of in-hospital mortality among CAD patients. SDI, SVI, and EJI demonstrated the strongest and most consistent associations. Researchers seeking to integrate area-level SDOH indices into predictive or risk-adjustment models should be aware of the indices’ components and select the most appropriate index.
Introduction
While risk prediction of cardiovascular outcomes, including in-hospital mortality, increasingly incorporates social determinants of health (SDOH), it remains unclear which area-level SDOH indices are most informative for predicting in-hospital mortality. Multiple area-level SDOH indices exist including the Social Vulnerability Index (SVI), Social Deprivation Index (SDI), Distressed Communities Index (DCI), Area Deprivation Index (ADI), Environmental Justice Index (EJI), Structural Racism Effect Index (SREI), and Community Deprivation Index (CDI).
Objective
The study aims to test the hypothesis that risk prediction of in-hospital mortality in patients with coronary artery disease may differ based on the specific SDOH index utilized.
Methods
We conducted a cohort study using data (2021-2023) from the Get with The Guidelines®–Coronary Artery Disease (GWTG-CAD) registry, linked to seven SDOH indices via patient’s residential ZIP code. For this linkage, Census tract-level SDOH indices were population-weighted to the ZIP code level. Correlations among indices were assessed using Pearson coefficients. To examine associations between each index and in-hospital mortality, generalized linear mixed models were used adjusting for potential confounders (e.g., age, sex, medical history and clinical presentation). Patients were categorized into quintiles using SDOH index (Q1 = least disadvantaged as reference, Q5 = most disadvantaged).
Results
Among 283,586 patients (median age 65 [IQR 18]; 33.3% female; 70.4% non-Hispanic White; 13.7% Black), correlations among the indices varied (r = 0.41–0.83), with strong correlations observed between SVI–EJI (r = 0.81) and SVI–CDI (r = 0.83). ADI showed weaker correlations (e.g., ADI–SDI r = 0.41; ADI–SVI r = 0.47)., Higher quintiles (greater social disadvantage) were generally associated with increased in-hospital mortality; but the strength and consistency varied among seven indices (Figure 1). SVI showed a clear and steady increase in mortality risk across quintiles, while ADI, SREI, and CDI had inconsistent relationships with in-hospital mortality.
Conclusions
Not all SDOH indices are equally predictive of in-hospital mortality among CAD patients. SDI, SVI, and EJI demonstrated the strongest and most consistent associations. Researchers seeking to integrate area-level SDOH indices into predictive or risk-adjustment models should be aware of the indices’ components and select the most appropriate index.
More abstracts on this topic:
3-Minute Heart Health App: A Feasibility Study
Abdulkarim Iya, Metzger Joseph, Stovitz Steven, Van't Hof Jeremy
A Focus for Improvement - Factors for Lab Adherence in a Pediatric Preventive Cardiology ProgramHolsinger Hunter, Porterfield Ronna, Taylor Makenna, Dresbach Bethany, Seipel Brittany, Igwe Chukwuemeka, Alvarado Chance, Tran Andrew