Final ID: MP1456
Older, non-White, Female and Uninsured Patients With a STEMI Are More Likely to be Transported to a non-Cardiac Cath Lab Center by EMS
Abstract Body (Do not enter title and authors here): Background:
For patients with ST segment elevation myocardial infarction (STEMI), rapid access to primary percutaneous coronary intervention (PPCI) is critical, and guidelines recommend communities create regional systems of care dedicated to reducing time to PPCI. Emergency medical services (EMS) transport of a patient with STEMI who lives near a hospital with a cardiac catheterization lab (CCL) to a hospital without a CCL represents a “system failure,” as it may delay PPCI.
Research Questions:
The study aimed to (1) assess the frequency and regional variability of EMS transport of patients with STEMI to a hospital without a CCL when a CCL was within a 60-minute drive (“system failure”); (2) compare demographic, socioeconomic, and clinical characteristics between patients with and without system failure; and (3) evaluate the association between system failure and time to PPCI.
Methods:
We analyzed data from the Get With The Guidelines- Coronary Artery Disease registry from January 1, 2020, to December 31, 2023. Adults with pre-hospital STEMI transported by ground EMS were included if they lived within 60 minutes of a CCL hospital. Patients were categorized as system failure (transport to non-CCL hospital) or no system failure (transport directly to CCL hospital). Baseline characteristics and in-hospital outcomes were compared between patients experiencing and not experiencing system failure, and generalized estimating equations adjusting for clinical, demographic, and hospital factors were used to evaluate associations between system failure status and treatment times.
Results:
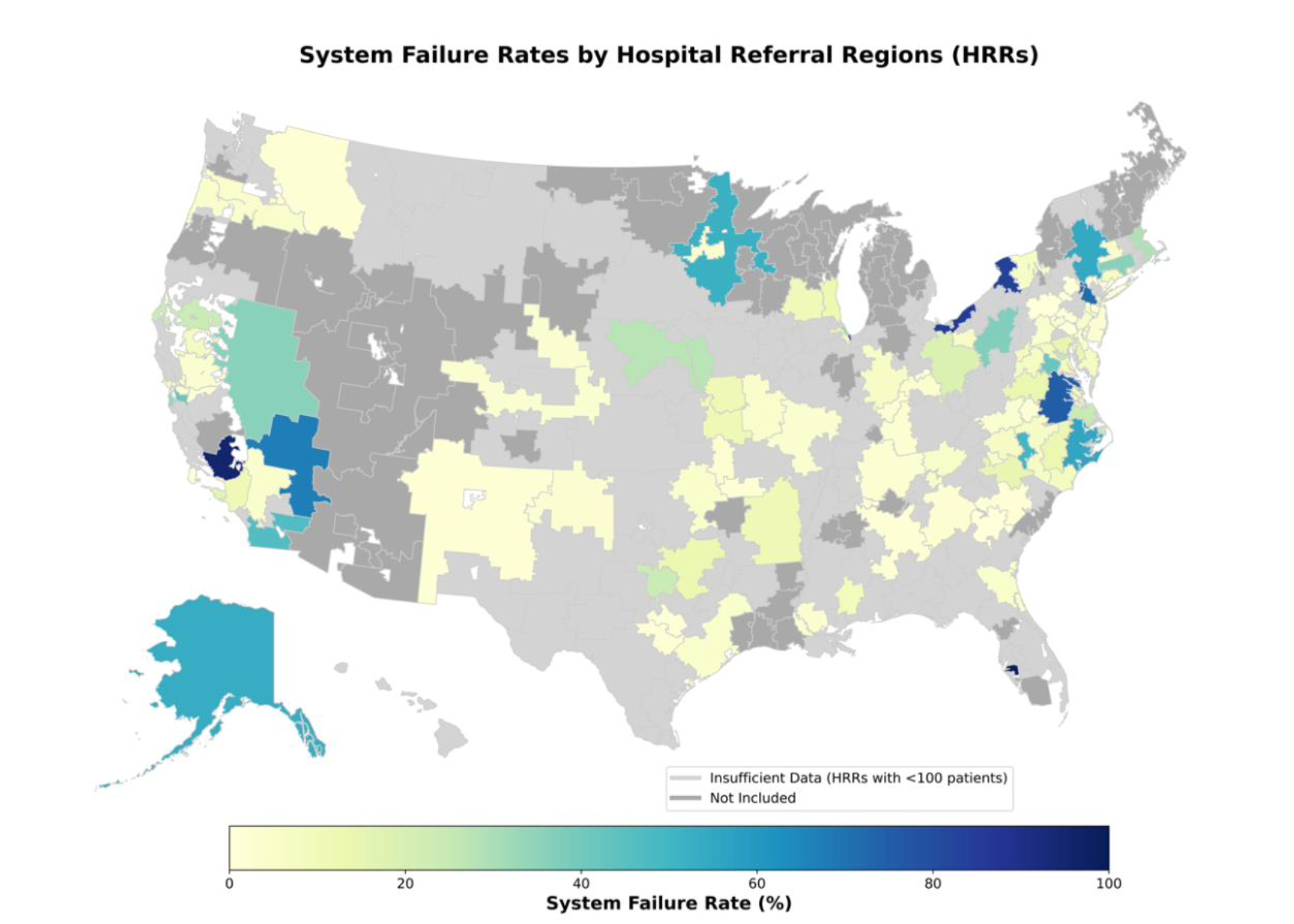
Of 46,741 patients with STEMI meeting inclusion criteria, 16% were transported to a hospital without a CCL. System failure rates varied widely across hospital referral regions (HRRs) (Figure 1). On multivariable analysis, patients experiencing system failure were more likely to be older, female, non-White, and be Medicaid-insured or uninsured (p < 0.01 for all comparisons). After adjustment, system failure was associated with significantly longer EMS First medical contact (FMC)-to-PCI times (+26 minutes; 95% CI, 10-42; p<0.001) and lower odds of achieving FMC-to-PCI time ≤ 90 minutes (OR 0.63; 95% CI 0.51-0.78, p<0.001).
Conclusions:
More than 1 in 6 STEMI patients living near CCL hospitals are transported to non-CCL hospitals, with resultant delays in timely reperfusion. Targeted efforts to optimize EMS transport protocols could improve timely access to reperfusion therapies.
For patients with ST segment elevation myocardial infarction (STEMI), rapid access to primary percutaneous coronary intervention (PPCI) is critical, and guidelines recommend communities create regional systems of care dedicated to reducing time to PPCI. Emergency medical services (EMS) transport of a patient with STEMI who lives near a hospital with a cardiac catheterization lab (CCL) to a hospital without a CCL represents a “system failure,” as it may delay PPCI.
Research Questions:
The study aimed to (1) assess the frequency and regional variability of EMS transport of patients with STEMI to a hospital without a CCL when a CCL was within a 60-minute drive (“system failure”); (2) compare demographic, socioeconomic, and clinical characteristics between patients with and without system failure; and (3) evaluate the association between system failure and time to PPCI.
Methods:
We analyzed data from the Get With The Guidelines- Coronary Artery Disease registry from January 1, 2020, to December 31, 2023. Adults with pre-hospital STEMI transported by ground EMS were included if they lived within 60 minutes of a CCL hospital. Patients were categorized as system failure (transport to non-CCL hospital) or no system failure (transport directly to CCL hospital). Baseline characteristics and in-hospital outcomes were compared between patients experiencing and not experiencing system failure, and generalized estimating equations adjusting for clinical, demographic, and hospital factors were used to evaluate associations between system failure status and treatment times.
Results:
Of 46,741 patients with STEMI meeting inclusion criteria, 16% were transported to a hospital without a CCL. System failure rates varied widely across hospital referral regions (HRRs) (Figure 1). On multivariable analysis, patients experiencing system failure were more likely to be older, female, non-White, and be Medicaid-insured or uninsured (p < 0.01 for all comparisons). After adjustment, system failure was associated with significantly longer EMS First medical contact (FMC)-to-PCI times (+26 minutes; 95% CI, 10-42; p<0.001) and lower odds of achieving FMC-to-PCI time ≤ 90 minutes (OR 0.63; 95% CI 0.51-0.78, p<0.001).
Conclusions:
More than 1 in 6 STEMI patients living near CCL hospitals are transported to non-CCL hospitals, with resultant delays in timely reperfusion. Targeted efforts to optimize EMS transport protocols could improve timely access to reperfusion therapies.
More abstracts on this topic:
Airway Opening Index is Associated with Return of Spontaneous Circulation in Swine and Humans with Cardiac Arrest
Bhandari Shiv, Coult Jason, Sharpe Zachary, Rea Thomas, Neumar Robert, Hsu Cindy, Counts Catherine, Sayre Michael, Johnson Nicholas
Ablation vs. Antiarrhythmic Drugs in Atrial Fibrillation: Real-World Treatment Gaps, Outcomes, and Equity ChallengesRauf Saman, Iqbal Fatima, Bhatti Shehzeen Dua, Masood Natasha, Qureshi Muhammad Maaz, Nawaz Muhammad Hassan