Final ID: MP2018
Left Atrial Passive Strain Rate by Cardiac Magnetic Resonance Imaging Better Reflects Left Ventricular Diastolic Function Than Left Atrial Reservoir Strain: A Cross-Sectional Study in a Post-COVID-19 Cohort
Abstract Body (Do not enter title and authors here): Introduction/Background: Left ventricular (LV) diastolic function is a key prognosticator in both disease and the general population. Given the physiological atrioventricular coupling, LV diastolic function is reflected in left atrial (LA) deformation. LA reservoir strain (LARS) is the most established index, despite being derived from the systolic phase, due to prior limitations in temporal resolution and reproducibility—now addressed with cardiac magnetic resonance imaging (CMR). Other LA indices may better reflect LV diastolic function than LARS.
Research questions/Hypothesis: To investigate LA strain indices by CMR and assess their association with LV diastolic function, compared to LARS.
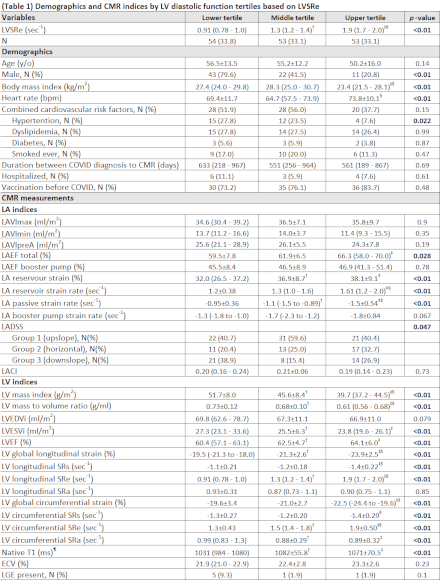
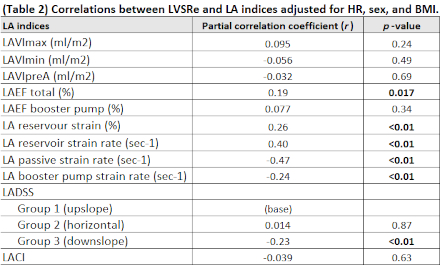
Methods/Approach: This preliminary cross-sectional analysis included patients post-COVID-19. Clinical and demographic data were extracted from medical records. CMR with CINE, T1 map, and late gadolinium enhancement (LGE) was performed on a 3T scanner (Canon Galan). CINE images were acquired with segmented bSSFP (FS=3), with reconstructed temporal resolution of ~25-33ms. Images were analyzed on a commercial workstation (Medis Suite 4.0.50.2). Demographic and CMR measures were summarized by tertiles of LV diastolic function, defined by LV maximum strain rate at early diastole (LVSRe). Correlations between LVSRe and LA indices were assessed, adjusting for demographics that differed across tertiles. Statistical significance was set at p<0.05.
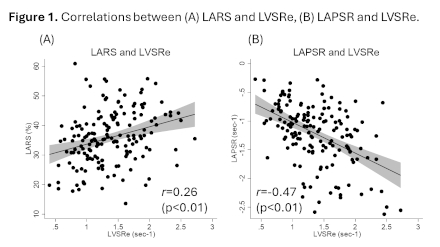
Results/Data: Overall, 160 participants with a median of ~20 months post-infection were included (Table 1). Better LV diastolic function was associated with female sex, lower body mass index (BMI), higher heart rate (HR), and enhanced LA and LV systolic and diastolic function, but not with LA volume, booster pump function, or the left atrioventricular coupling index (LACI). LARS did not differ between the middle and upper tertiles, whereas LA passive SR (LAPSR) differed significantly across all tertiles. The correlation between LVSRe and LAPSR, adjusted for sex, BMI, and HR, was stronger than with LARS (r = -0.47 and r = 0.26, both p<0.01) (Table 2, Figure 1); these trends remained after further adjusting for age and cardiac comorbidities.
Conclusions: LAPSR is a better indicator of LV diastolic function than LARS, consistent with its physiological role as a diastolic-phase index and counterpart to LVSRe. Advances in CMR support the utility of LA indices beyond LARS.
Research questions/Hypothesis: To investigate LA strain indices by CMR and assess their association with LV diastolic function, compared to LARS.
Methods/Approach: This preliminary cross-sectional analysis included patients post-COVID-19. Clinical and demographic data were extracted from medical records. CMR with CINE, T1 map, and late gadolinium enhancement (LGE) was performed on a 3T scanner (Canon Galan). CINE images were acquired with segmented bSSFP (FS=3), with reconstructed temporal resolution of ~25-33ms. Images were analyzed on a commercial workstation (Medis Suite 4.0.50.2). Demographic and CMR measures were summarized by tertiles of LV diastolic function, defined by LV maximum strain rate at early diastole (LVSRe). Correlations between LVSRe and LA indices were assessed, adjusting for demographics that differed across tertiles. Statistical significance was set at p<0.05.
Results/Data: Overall, 160 participants with a median of ~20 months post-infection were included (Table 1). Better LV diastolic function was associated with female sex, lower body mass index (BMI), higher heart rate (HR), and enhanced LA and LV systolic and diastolic function, but not with LA volume, booster pump function, or the left atrioventricular coupling index (LACI). LARS did not differ between the middle and upper tertiles, whereas LA passive SR (LAPSR) differed significantly across all tertiles. The correlation between LVSRe and LAPSR, adjusted for sex, BMI, and HR, was stronger than with LARS (r = -0.47 and r = 0.26, both p<0.01) (Table 2, Figure 1); these trends remained after further adjusting for age and cardiac comorbidities.
Conclusions: LAPSR is a better indicator of LV diastolic function than LARS, consistent with its physiological role as a diastolic-phase index and counterpart to LVSRe. Advances in CMR support the utility of LA indices beyond LARS.
More abstracts on this topic:
A mechanism whereby SGLT2 inhibitor dapagliflozin reverses cardiac diastolic dysfunction in a model of HFpEF
Liu Man, Liu Hong, Kang Gyeoung-jin, Kim Eunji, Neumann Mitchell, Johnson Madeline, Murikinati Ruthvika, Dudley Samuel
Atrial Cardiopathy Biomarkers and Brain Infarction in Multiple Territories in ARCADIAGologorsky Rachel, Karunamuni Nilushi, Longstreth W, Tirschwell David, Elkind Mitchell, Kamel Hooman