Final ID: MP936
Unaffected Carriers of a Pathogenic BMPR2 Variant Exhibit a Distinct Cytokine Signature Associated with Subclinical Changes on Right Ventricular and Pulmonary Vascular Imaging
Abstract Body (Do not enter title and authors here): Introduction: Pathogenic BMPR2 variants are a major genetic risk factor for pulmonary arterial hypertension (PAH), though the disease shows incomplete penetrance, suggesting that additional modifiers influence diease onset. While cytokine profiles are altered in PAH, it remains unclear whether unaffected carriers (UCs) of pathogenic BMPR2 variants exhibit a distinct immune signature.
Hypothesis: We hypothesized that UCs of pathogenic BMPR2 variants display a distinct cytokine profile compared to non-carrier controls.
Methods:Blood samples were collected from 23 UCs and 13 healthy controls as part of a prospective longitudinal cohort study (DOLPHIN-GENESIS). Circulating cytokine levels were quantified using Luminex panels. UCs also underwent cardiac magnetic resonance imaging (MRI), transthoracic echocardiography (TTE), and right heart catheterization (RHC). Group comparisons were performed using Wilcoxon rank-sum tests with Benjamini-Hochberg correction to adjust for multiple comparisons.
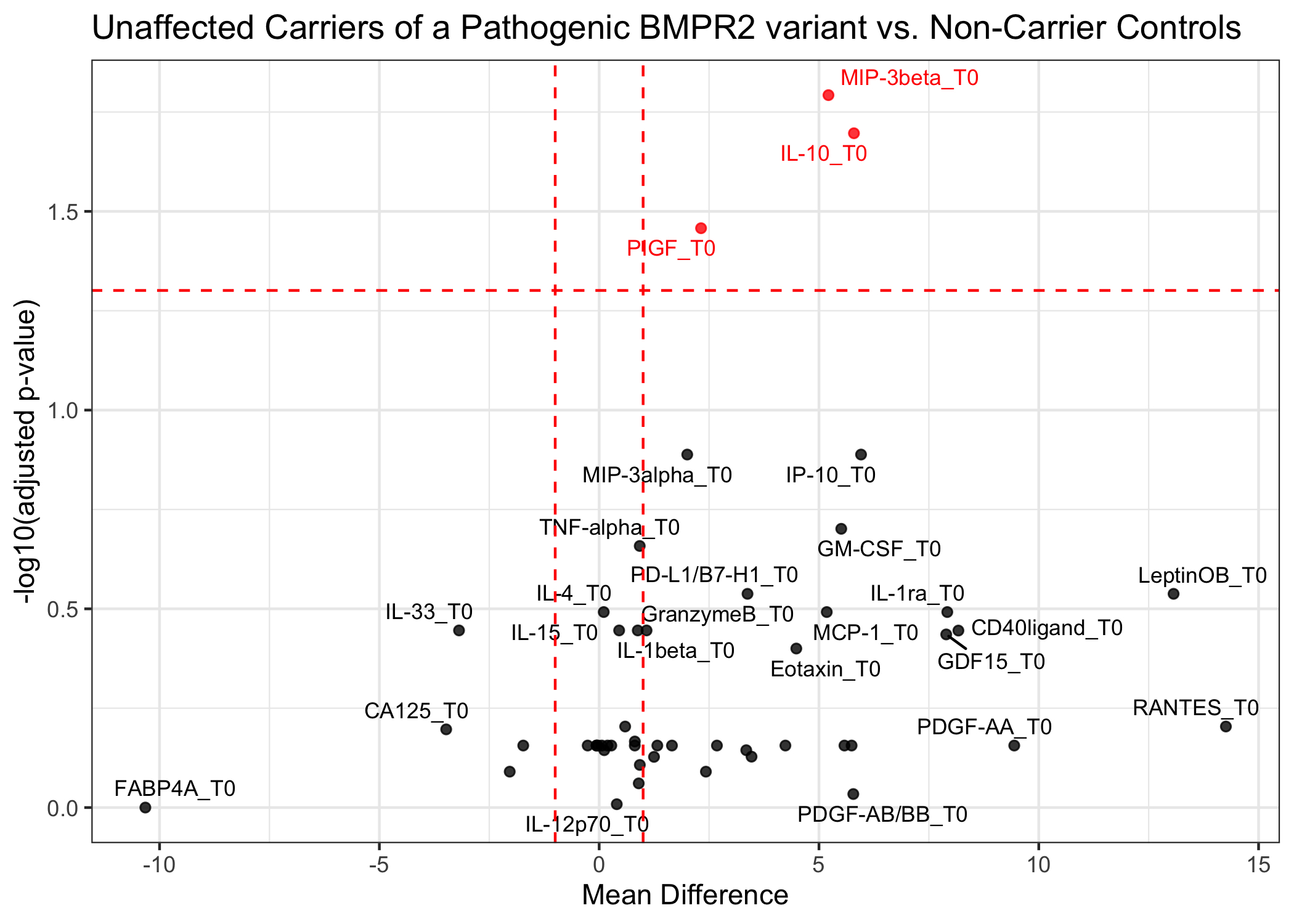
Results: Compared to controls, UCs had elevated levels of pro-inflammatory placental growth factor (PlGF) (Control: 4.4 pg/mL vs. UC: 8.4 pg/mL; p=0.018) and macrophage inflammatory protein-3β (MIP-3β) (Control: 3.2 pg/mL vs. UC: 6.8 pg/mL; p=0.004), as well as anti-inflammatory interleukin-10 (IL-10) (Control: 3.0 pg/mL vs. UC: 8.5 pg/mL; p=0.008). PlGF correlated positively with RHC-derived systolic pulmonary artery pressure (r=0.57, p=0.011) and negatively with pulmonary artery acceleration time on TTE (r=−0.41, p=0.028). IL-10 and MIP-3β both showed negative correlations with right ventricular (RV) end-systolic (IL-10: r=−0.4, p=0.016; MIP-3β: r=−0.4, p=0.017) and end-diastolic (IL-10: r=−0.42; MIP-3β: r=−0.43, p=0.009) volumes, as well as RV mass (IL-10: r=−0.39, p=0.020; MIP-3β: r=−0.41, p=0.015).
Conclusion: UCs of a pathogenic BMPR2 variant display a distinct inflammatory profile despite the absence of disease. Elevated MIP-3β, a chemokine involved in T-cell and macrophage-precursor recruitment, and IL-10, an anti-inflammatory cytokine closely regulating MIP-3β, were observed. PlGF, an angiogenic factor promoting cytokine production, was also increased. These cytokine alterations was associated with subtle changes in pulmonary vascular and right ventricular parameters on imaging. Ongoing analyses aim to clarify how these immune shifts affect interactions between macrophages, endothelial cells, and cardiomyocytes in unaffected carriers of a pathogenic BMPR2 variant.
Hypothesis: We hypothesized that UCs of pathogenic BMPR2 variants display a distinct cytokine profile compared to non-carrier controls.
Methods:Blood samples were collected from 23 UCs and 13 healthy controls as part of a prospective longitudinal cohort study (DOLPHIN-GENESIS). Circulating cytokine levels were quantified using Luminex panels. UCs also underwent cardiac magnetic resonance imaging (MRI), transthoracic echocardiography (TTE), and right heart catheterization (RHC). Group comparisons were performed using Wilcoxon rank-sum tests with Benjamini-Hochberg correction to adjust for multiple comparisons.
Results: Compared to controls, UCs had elevated levels of pro-inflammatory placental growth factor (PlGF) (Control: 4.4 pg/mL vs. UC: 8.4 pg/mL; p=0.018) and macrophage inflammatory protein-3β (MIP-3β) (Control: 3.2 pg/mL vs. UC: 6.8 pg/mL; p=0.004), as well as anti-inflammatory interleukin-10 (IL-10) (Control: 3.0 pg/mL vs. UC: 8.5 pg/mL; p=0.008). PlGF correlated positively with RHC-derived systolic pulmonary artery pressure (r=0.57, p=0.011) and negatively with pulmonary artery acceleration time on TTE (r=−0.41, p=0.028). IL-10 and MIP-3β both showed negative correlations with right ventricular (RV) end-systolic (IL-10: r=−0.4, p=0.016; MIP-3β: r=−0.4, p=0.017) and end-diastolic (IL-10: r=−0.42; MIP-3β: r=−0.43, p=0.009) volumes, as well as RV mass (IL-10: r=−0.39, p=0.020; MIP-3β: r=−0.41, p=0.015).
Conclusion: UCs of a pathogenic BMPR2 variant display a distinct inflammatory profile despite the absence of disease. Elevated MIP-3β, a chemokine involved in T-cell and macrophage-precursor recruitment, and IL-10, an anti-inflammatory cytokine closely regulating MIP-3β, were observed. PlGF, an angiogenic factor promoting cytokine production, was also increased. These cytokine alterations was associated with subtle changes in pulmonary vascular and right ventricular parameters on imaging. Ongoing analyses aim to clarify how these immune shifts affect interactions between macrophages, endothelial cells, and cardiomyocytes in unaffected carriers of a pathogenic BMPR2 variant.
More abstracts on this topic:
4D Cardiac Magnetic Resonance Identifies Differences in Regional Strain Patterns Among Pediatric Heart Transplant Patients with Acute Rejection or Cardiac Allograft Vasculopathy
Henderson Christopher, Starnes Joseph, Samyn Margaret, Damon Bruce, Hernandez Lazaro, Goergen Craig, Soslow Jonathan, Prado Marco Aurélio, Earl Conner, Georgedurrett Kristen, Lee Simon, Nandi Deipanjan, Chan Kak-chen, Shugh Svetlana, Kikano Sandra
3D Statistical Shape Analysis Predicts Type A Aortic Dissection Better Than Aortic DiametersMarway Prabhvir, Campello Jorge Carlos Alberto, Wagner Catherine, Baker Timothy, Burris Nicholas