Final ID: Su2110
Food Insecurity Drives Obesity: Highlighting the Hunger–Obesity Paradox Across the United States
Abstract Body (Do not enter title and authors here): Background:
Obesity-related cardiovascular death rates in the U.S. have nearly tripled over the past two decades, rising from 2.2 to 6.6 deaths per 100,000 people, highlighting a growing public health crisis that demands urgent attention. The hunger–obesity paradox occurs when limited access to nutritious food forces individuals to rely on inexpensive, calorie-dense alternatives, leading to higher obesity rates despite food scarcity.
Objective:
We aim to understand the influence of social determinants of health, specifically food insecurity, poverty, and educational attainment, on obesity prevalence rates across the 50 states in the United States. We seek to identify the variables that contribute to disparities in obesity prevalence and to propose state-specific public health strategies. Additionally, we aim to shed light on the hunger–obesity paradox by focusing on the role of the food insecurity index in influencing obesity prevalence rates.
Methods:
We analyzed state-level data from 2023 obtained from the Centers for Disease Control and Prevention (CDC) and the U.S. Census Bureau. Descriptive statistics and Pearson correlations were used to assess the associations between obesity and key variables. A multivariate linear regression model was then employed to evaluate the independent effects of these variables on state-level obesity prevalence.
Results
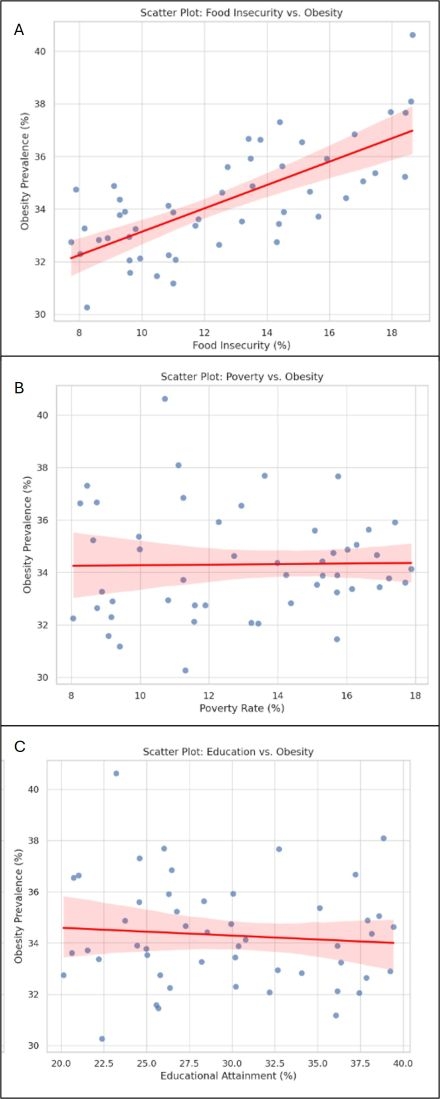
Across the 50 states, the average obesity prevalence was 36.48%, ranging from 30.1% in Florida to 42.4% in Oklahoma. The average food insecurity rate was 11.79%, with the highest observed in Arkansas (18.9%) and the lowest in New Hampshire (7.4%). Food insecurity demonstrated the strongest positive correlation with obesity prevalence (r = 0.48, p < 0.001), followed by poverty (r = 0.27, p = 0.062). Educational attainment showed a weak, non-significant inverse correlation (r = –0.10, p = 0.48).
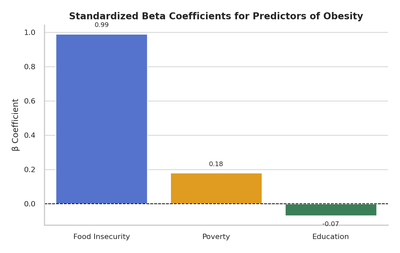
In the multivariate regression model, food insecurity, poverty, and education collectively explained 31.6% of the variance in state-level obesity rates (adjusted R^2 = 0.316, p = 0.0005). Notably, food insecurity remained the only statistically significant independent predictor of obesity prevalence (β = 0.99, p < 0.001).
Conclusion:
Food insecurity is a key driver of obesity prevalence, independent of poverty and education. This highlights the importance of ensuring equitable access to nutritious food as part of public health efforts to reduce obesity-related complications and health disparities.
Obesity-related cardiovascular death rates in the U.S. have nearly tripled over the past two decades, rising from 2.2 to 6.6 deaths per 100,000 people, highlighting a growing public health crisis that demands urgent attention. The hunger–obesity paradox occurs when limited access to nutritious food forces individuals to rely on inexpensive, calorie-dense alternatives, leading to higher obesity rates despite food scarcity.
Objective:
We aim to understand the influence of social determinants of health, specifically food insecurity, poverty, and educational attainment, on obesity prevalence rates across the 50 states in the United States. We seek to identify the variables that contribute to disparities in obesity prevalence and to propose state-specific public health strategies. Additionally, we aim to shed light on the hunger–obesity paradox by focusing on the role of the food insecurity index in influencing obesity prevalence rates.
Methods:
We analyzed state-level data from 2023 obtained from the Centers for Disease Control and Prevention (CDC) and the U.S. Census Bureau. Descriptive statistics and Pearson correlations were used to assess the associations between obesity and key variables. A multivariate linear regression model was then employed to evaluate the independent effects of these variables on state-level obesity prevalence.
Results
Across the 50 states, the average obesity prevalence was 36.48%, ranging from 30.1% in Florida to 42.4% in Oklahoma. The average food insecurity rate was 11.79%, with the highest observed in Arkansas (18.9%) and the lowest in New Hampshire (7.4%). Food insecurity demonstrated the strongest positive correlation with obesity prevalence (r = 0.48, p < 0.001), followed by poverty (r = 0.27, p = 0.062). Educational attainment showed a weak, non-significant inverse correlation (r = –0.10, p = 0.48).
In the multivariate regression model, food insecurity, poverty, and education collectively explained 31.6% of the variance in state-level obesity rates (adjusted R^2 = 0.316, p = 0.0005). Notably, food insecurity remained the only statistically significant independent predictor of obesity prevalence (β = 0.99, p < 0.001).
Conclusion:
Food insecurity is a key driver of obesity prevalence, independent of poverty and education. This highlights the importance of ensuring equitable access to nutritious food as part of public health efforts to reduce obesity-related complications and health disparities.
More abstracts on this topic:
A Novel Composite Artificial Intelligence-Electrocardiography Risk Score Is Independently Associated with Mortality in Chronic Tricuspid Regurgitation
Ciobanu Andrea, Pellikka Patricia, Kane Garvan, Pislaru Sorin, Anand Vidhu, Naser Jwan, Wood Julia, Friedman Paul, Vinereanu Dragos, Nkomo Vuyisile, Pislaru Cristina, Lara-breitinger Kyla, Thaden Jeremy
Disaggregating Cardiovascular-Kidney-Metabolic Mortality among Asian Subgroups in the United StatesSaleem Hira, Shahid Izza, Dong Weichuan, Nasir Khurram, Al-kindi Sadeer