Final ID: MP1314
Rural-Urban Disparities in Cardiovascular Mortality Among Chemotherapy-Treated Cancer Survivors: A SEER-Based Analysis
Abstract Body (Do not enter title and authors here): Background:
Cardiovascular disease (CVD) is the leading non-cancer cause of mortality among cancer survivors, with rural populations facing systemic disparities in access to cardio-oncology care. We hypothesized that cardiovascular mortality is disproportionately higher among rural cancer survivors and sought to quantify these disparities using SEER data.
Methods:
Using Surveillance, Epidemiology, and End Results (SEER) data from 2000 to 2021, we conducted a retrospective cohort study of 1,458,583 deceased cancer patients who had received chemotherapy, as indicated by SEER treatment records coded for “Yes” in the chemotherapy received variable. Rurality was defined using Rural-Urban Continuum Codes (RUCC), distinguishing nonmetropolitan, non-adjacent counties from large metropolitan areas (≥1 million population). Cardiovascular disease mortality, defined as the primary cause of death using SEER cause-of-death codes, was identified in 71,892 patients. Relative risks (RR) were calculated (unadjusted), and rural-urban disparities were assessed using chi-square tests.
Results:
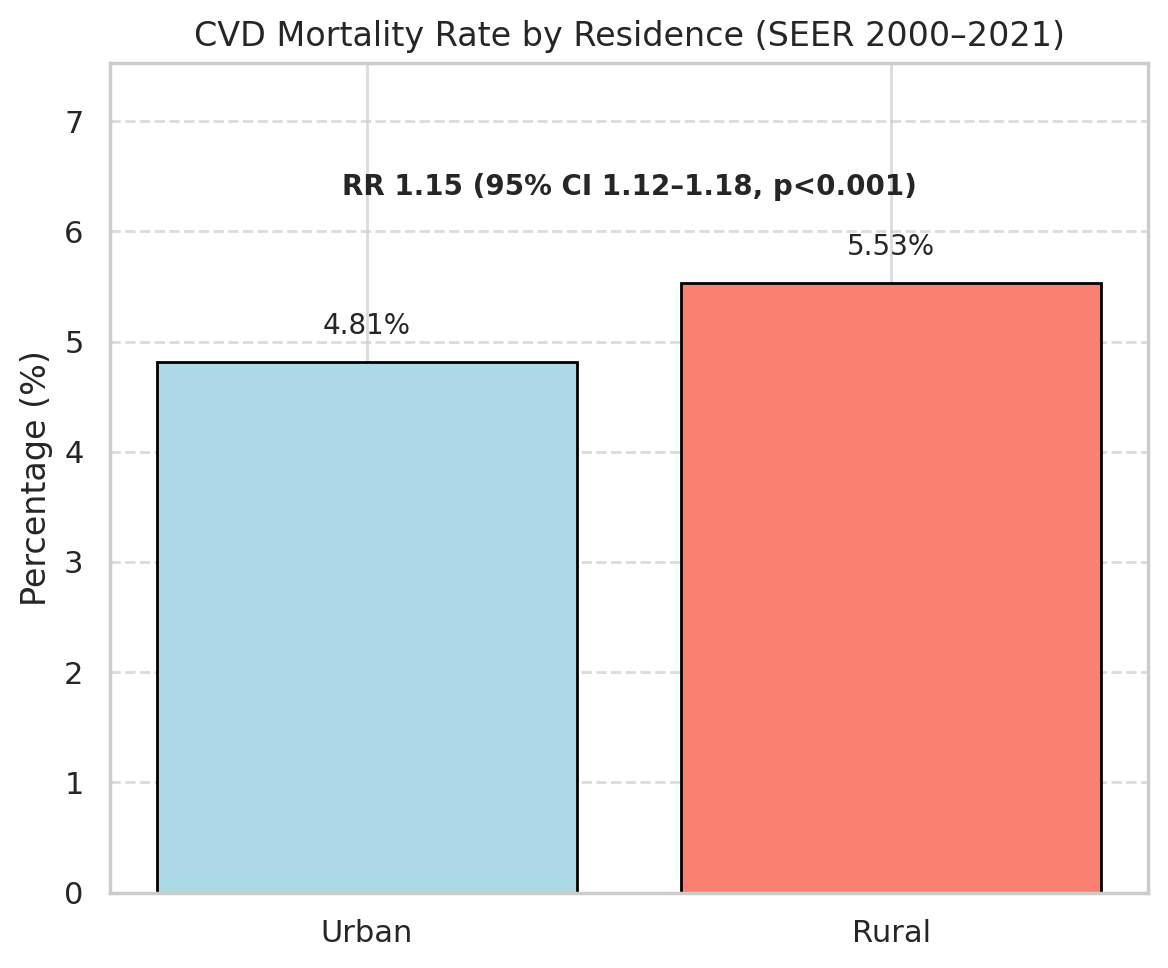
Patients residing in rural, nonmetropolitan, non-adjacent counties had higher cardiovascular disease mortality (Rural: 5.53%, Urban: 4.81%). This represented a 15% increased proportional risk (RR 1.15, 95% CI 1.12–1.18, p<0.001). Heart diseases accounted for 92% of all cardiovascular deaths, with a slightly higher proportion in rural areas (93.2%) compared to urban areas (91.6%). Hypertension-related deaths were more prevalent in urban patients (Urban: 4.9%, Rural: 3.3%), which may reflect geographic variation in comorbidities or diagnostic coding practices.
Conclusion:
Rural residence is independently associated with increased cardiovascular disease mortality among chemotherapy-treated cancer survivors. Contributing factors may include limited access to specialty care, higher baseline cardiovascular risk, and fragmented survivorship monitoring in rural settings. These findings highlight the need for targeted interventions, such as expanding telehealth services, developing rural-specific survivorship guidelines, and policy reforms to improve access to cardio-oncology care. Limitations include the lack of detailed treatment data and unmeasured confounders inherent to SEER. Future research should focus on optimizing care delivery models and integrating geographic risk stratification into survivorship care planning.
Cardiovascular disease (CVD) is the leading non-cancer cause of mortality among cancer survivors, with rural populations facing systemic disparities in access to cardio-oncology care. We hypothesized that cardiovascular mortality is disproportionately higher among rural cancer survivors and sought to quantify these disparities using SEER data.
Methods:
Using Surveillance, Epidemiology, and End Results (SEER) data from 2000 to 2021, we conducted a retrospective cohort study of 1,458,583 deceased cancer patients who had received chemotherapy, as indicated by SEER treatment records coded for “Yes” in the chemotherapy received variable. Rurality was defined using Rural-Urban Continuum Codes (RUCC), distinguishing nonmetropolitan, non-adjacent counties from large metropolitan areas (≥1 million population). Cardiovascular disease mortality, defined as the primary cause of death using SEER cause-of-death codes, was identified in 71,892 patients. Relative risks (RR) were calculated (unadjusted), and rural-urban disparities were assessed using chi-square tests.
Results:
Patients residing in rural, nonmetropolitan, non-adjacent counties had higher cardiovascular disease mortality (Rural: 5.53%, Urban: 4.81%). This represented a 15% increased proportional risk (RR 1.15, 95% CI 1.12–1.18, p<0.001). Heart diseases accounted for 92% of all cardiovascular deaths, with a slightly higher proportion in rural areas (93.2%) compared to urban areas (91.6%). Hypertension-related deaths were more prevalent in urban patients (Urban: 4.9%, Rural: 3.3%), which may reflect geographic variation in comorbidities or diagnostic coding practices.
Conclusion:
Rural residence is independently associated with increased cardiovascular disease mortality among chemotherapy-treated cancer survivors. Contributing factors may include limited access to specialty care, higher baseline cardiovascular risk, and fragmented survivorship monitoring in rural settings. These findings highlight the need for targeted interventions, such as expanding telehealth services, developing rural-specific survivorship guidelines, and policy reforms to improve access to cardio-oncology care. Limitations include the lack of detailed treatment data and unmeasured confounders inherent to SEER. Future research should focus on optimizing care delivery models and integrating geographic risk stratification into survivorship care planning.
More abstracts on this topic:
Activated CD8+HLA-DR+ T Cells as Immune Biomarkers of Metabolic Dysfunction and Cardiovascular Risk in Prediabetes
Alrashed Fatema, Alsaeed Halemah, Alturaiki Wael, Akhter Nadeem, Alosaimi Bandar, Almutairi Saeedah, Mubarak Ayman, Al-mulla Fahd, Ahmad Rasheed
A Machine Learning-Derived Socio-Environmental Risk Score More Accurately Predicts Cardiovascular Events and Better Addresses Health Inequities than Social Deprivation IndexChen Zhuo, Nasir Khurram, Al-kindi Sadeer, Rajagopalan Sanjay, Ponnana Sai Rahul, Dazard Jean-eudes, Zhang Tong, Dong Weichuan, Okyere Robert, Sirasapalli Santosh, Deo Salil, Khraishah Haitham