Final ID: Mo3115
Differential Outcomes of TAVR With and Without Percutaneous Coronary Intervention During Same Hospitalization
Abstract Body (Do not enter title and authors here): Background: Transcatheter aortic valve replacement (TAVR) has emerged as a transformative, minimally invasive alternative to surgical aortic valve replacement for patients with trileaflet aortic stenosis. While the use of TAVR continues to expand, limited data exist regarding contemporary trends and clinical outcomes associated with TAVR with and without percutaneous coronary intervention (PCI) during the same hospitalization.
Methods: The National Inpatient Sample database from 2018 to 2022 was used, and regression analysis was performed.
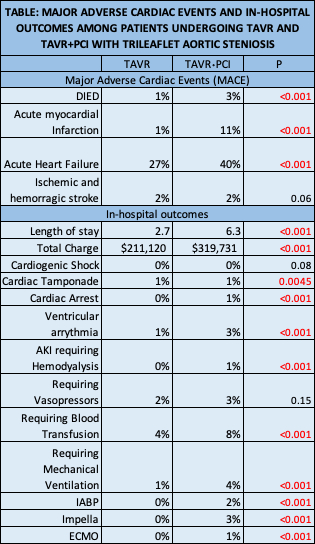
Results: Among 323,785 patients with a primary diagnosis of aortic stenosis and a history of coronary artery disease, 211,125 (65.2%) underwent TAVR alone (TAVR), while 5,900 (1.8%) underwent TAVR and PCI (TAVR+PCI) during the same index hospitalization. Compared to TAVR only group, patients in the TAVR+PCI group were more often female (43% vs 37%, p<0.001), less often White (83% vs 88%, p=0.0001), and more often in the highest income quartile (76th–100th percentile: 30% vs 26%, p=0.03). The prevalence of Charlson Comorbidity Index ≥3 was comparable between groups (57% vs 54%, p=0.25), and no significant age difference was observed. Multivariable logistic regression identified the Charlson Comorbidity Index ≥3 as an independent predictor of in-hospital mortality. Adjusted analyses revealed that the TAVR+PCI group had a higher incidence of major adverse cardiovascular events (MACE), including in-hospital mortality (3% vs 1%, p<0.001), acute myocardial infarction (11% vs 1%, p<0.001), and acute heart failure (40% vs 27%, p<0.001) although, stroke rates, both ischemic and hemorrhagic, were similar between 2 groups (2% vs 2%, p=0.06). Patients undergoing TAVR+PCI experienced longer hospital stays (mean 6.3 vs 2.7 days, p<0.001) and incurred higher hospitalization costs (mean $319,731 vs $211,120, p<0.001) compared to those undergoing TAVR alone. This study also showed TAVR+PCI group suffered more adverse in-hospital outcomes compared to TAVR only group [Table].
Conclusion: This study indicates that concomitant TAVR and PCI is associated with higher rates of mortality, acute myocardial infarction, and heart failure compared to TAVR alone. Other studies have indicated that the strategy of performing PCI within 90 days prior to TAVR may mitigate such adverse outcomes.
Methods: The National Inpatient Sample database from 2018 to 2022 was used, and regression analysis was performed.
Results: Among 323,785 patients with a primary diagnosis of aortic stenosis and a history of coronary artery disease, 211,125 (65.2%) underwent TAVR alone (TAVR), while 5,900 (1.8%) underwent TAVR and PCI (TAVR+PCI) during the same index hospitalization. Compared to TAVR only group, patients in the TAVR+PCI group were more often female (43% vs 37%, p<0.001), less often White (83% vs 88%, p=0.0001), and more often in the highest income quartile (76th–100th percentile: 30% vs 26%, p=0.03). The prevalence of Charlson Comorbidity Index ≥3 was comparable between groups (57% vs 54%, p=0.25), and no significant age difference was observed. Multivariable logistic regression identified the Charlson Comorbidity Index ≥3 as an independent predictor of in-hospital mortality. Adjusted analyses revealed that the TAVR+PCI group had a higher incidence of major adverse cardiovascular events (MACE), including in-hospital mortality (3% vs 1%, p<0.001), acute myocardial infarction (11% vs 1%, p<0.001), and acute heart failure (40% vs 27%, p<0.001) although, stroke rates, both ischemic and hemorrhagic, were similar between 2 groups (2% vs 2%, p=0.06). Patients undergoing TAVR+PCI experienced longer hospital stays (mean 6.3 vs 2.7 days, p<0.001) and incurred higher hospitalization costs (mean $319,731 vs $211,120, p<0.001) compared to those undergoing TAVR alone. This study also showed TAVR+PCI group suffered more adverse in-hospital outcomes compared to TAVR only group [Table].
Conclusion: This study indicates that concomitant TAVR and PCI is associated with higher rates of mortality, acute myocardial infarction, and heart failure compared to TAVR alone. Other studies have indicated that the strategy of performing PCI within 90 days prior to TAVR may mitigate such adverse outcomes.
More abstracts on this topic:
Cellular retention of growth arrest specific protein 6 (GAS6) accelerates calcification of aortic valves
Turner Mandy, Aikawa Elena, Itoh Shinsuke, Hoekstra Joost, Blaser Mark, Mikami Kentaro, Clift Cassandra, Muehlschlegel Jochen, Singh Sasha, Aikawa Masanori
A Meta-Analysis Comparing Same-Day Discharge to Later-Day Discharge in Transcatheter Aortic Valve ReplacementJain Hritvik, Passey Siddhant, Jain Jyoti, Goyal Aman, Wasir Amanpreet, Ahmed Mushood, Patel Nandan, Yadav Ashish, Shah Janhvi, Mehta Aryan