Final ID: MP1031
Peripheral Artery Disease and Post-Transplant Outcomes: Disease Burden Overcomes Distribution
Abstract Body (Do not enter title and authors here): Introduction: Peripheral artery disease (PAD) is a known risk factor for adverse cardiovascular outcomes and has historically been viewed as a relative contraindication to heart transplantation (HT). However, as management of PAD improves and transplant eligibility broadens, the impact of PAD on post-HT outcomes warrants reevaluation.
Hypothesis: Pre-HT PAD, driven by extremity PAD, is associated with increased risk of 1-year post-HT adverse outcomes, including all-cause mortality, cerebrovascular accident (CVA), renal replacement therapy (RRT), graft dysfunction, and adverse vascular outcomes.
Methods: We conducted a retrospective cohort study of patients who underwent HT at a large, advanced heart failure center from January 2012 to May 2022. PAD was defined by history of CVA, claudication, abnormal ankle-brachial index (ABI <1), abnormal carotid dopplers (>50% stenosis), or abnormal upper or lower extremity arterial dopplers (>50% stenosis). Patients were stratified by PAD status and subtype: central/cerebrovascular (CVA or abnormal carotid dopplers) and extremity (claudication, abnormal ABI, or abnormal extremity dopplers). Outcomes included 1-year all-cause mortality, CVA, RRT, graft dysfunction (ejection fraction <55%), and vascular complications (consults or abnormal imaging). Group comparisons used multivariable logistic regression adjusted for PAD subtype using Python®.
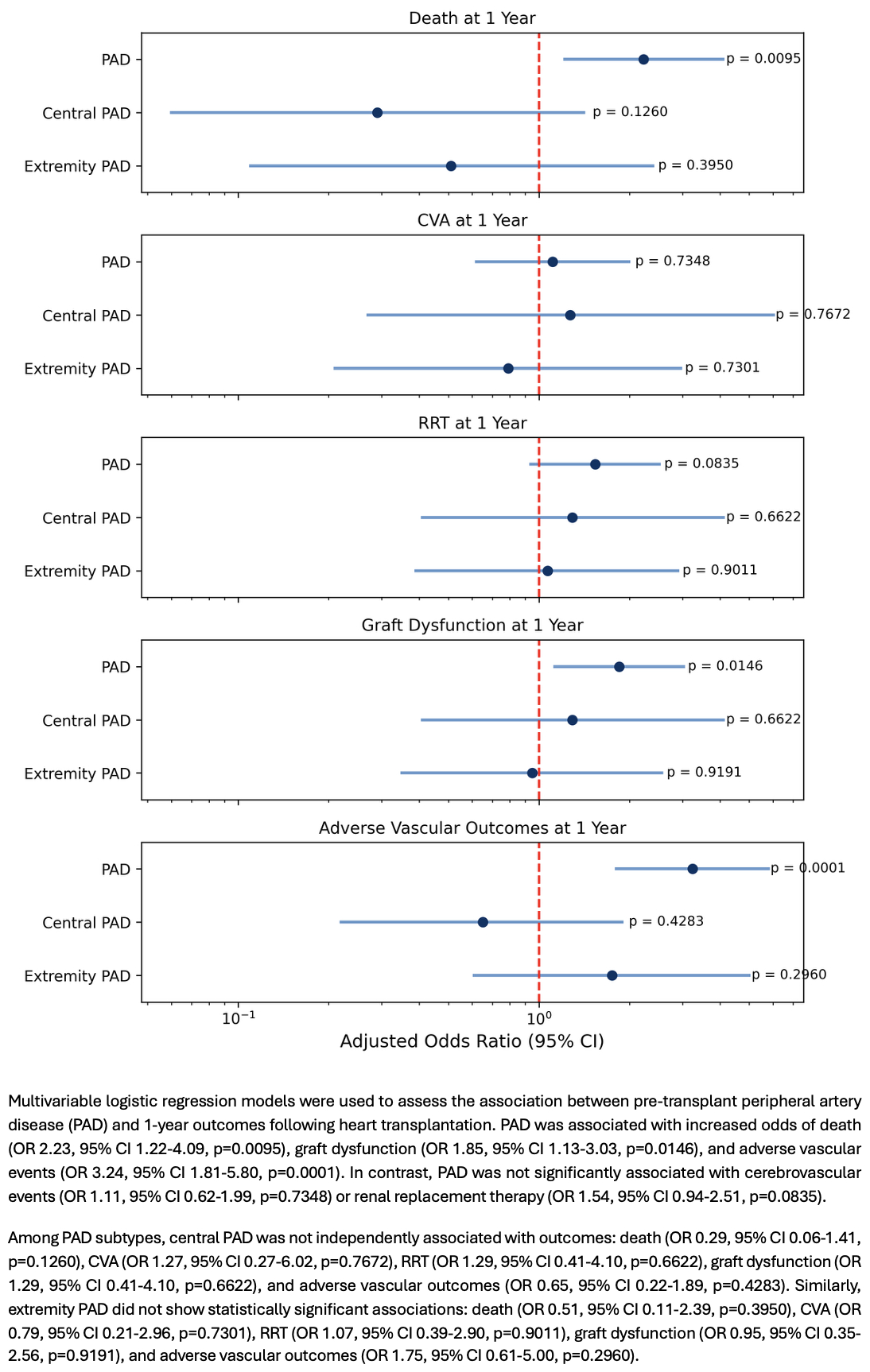
Results: Of the 595 patients (mean age 53 years; 28% female; 27% Black), 216 (36%) had PAD. The PAD group exhibited higher rates of pre-HT diabetes (32% vs 21%, p<0.01) and hypertension (58% vs 44%, p<0.01). No significant differences in age, sex, race, kidney disease, or smoking were found between groups. In the PAD group, one-year all-cause mortality was more than double those without PAD (11.6% vs 5.5%, p=0.01). Graft dysfunction was also higher (16.7% vs 9.8%, p=0.02), while CVA (9.3% vs 8.4%, p=0.85) and RRT (15.7% vs 10.8%, p=0.11) were not significantly different in PAD patients compared to those without. PAD patients also had increased vascular complications at 1 year (15.3% vs 5.3%, p<0.001). However, when stratified by PAD subtype, neither central/cerebrovascular nor extremity PAD independently predicted outcomes (Figure).
Conclusion: Total PAD burden pre-HT was associated with increased all-cause mortality, graft dysfunction, and vascular complications at 1 year. These findings underscore the importance of incorporating PAD into pre- and post-HT management.
Hypothesis: Pre-HT PAD, driven by extremity PAD, is associated with increased risk of 1-year post-HT adverse outcomes, including all-cause mortality, cerebrovascular accident (CVA), renal replacement therapy (RRT), graft dysfunction, and adverse vascular outcomes.
Methods: We conducted a retrospective cohort study of patients who underwent HT at a large, advanced heart failure center from January 2012 to May 2022. PAD was defined by history of CVA, claudication, abnormal ankle-brachial index (ABI <1), abnormal carotid dopplers (>50% stenosis), or abnormal upper or lower extremity arterial dopplers (>50% stenosis). Patients were stratified by PAD status and subtype: central/cerebrovascular (CVA or abnormal carotid dopplers) and extremity (claudication, abnormal ABI, or abnormal extremity dopplers). Outcomes included 1-year all-cause mortality, CVA, RRT, graft dysfunction (ejection fraction <55%), and vascular complications (consults or abnormal imaging). Group comparisons used multivariable logistic regression adjusted for PAD subtype using Python®.
Results: Of the 595 patients (mean age 53 years; 28% female; 27% Black), 216 (36%) had PAD. The PAD group exhibited higher rates of pre-HT diabetes (32% vs 21%, p<0.01) and hypertension (58% vs 44%, p<0.01). No significant differences in age, sex, race, kidney disease, or smoking were found between groups. In the PAD group, one-year all-cause mortality was more than double those without PAD (11.6% vs 5.5%, p=0.01). Graft dysfunction was also higher (16.7% vs 9.8%, p=0.02), while CVA (9.3% vs 8.4%, p=0.85) and RRT (15.7% vs 10.8%, p=0.11) were not significantly different in PAD patients compared to those without. PAD patients also had increased vascular complications at 1 year (15.3% vs 5.3%, p<0.001). However, when stratified by PAD subtype, neither central/cerebrovascular nor extremity PAD independently predicted outcomes (Figure).
Conclusion: Total PAD burden pre-HT was associated with increased all-cause mortality, graft dysfunction, and vascular complications at 1 year. These findings underscore the importance of incorporating PAD into pre- and post-HT management.
More abstracts on this topic:
Aging Alone: Impact of Social Networks on Older Adults with Advanced Heart Failure
Godfrey Sarah, Drazner Mark, Farr Maryjane, Jawaid Anas, Maini Mansi, Zhang Jingwen, Dutta Manasa, Wrobel Christopher, Thibodeau Jennifer, Grodin Justin, Morlend Robert
Allograft Outcomes of Adding Proprotein Convertase Subtilisin Kexin 9 Inhibitors or Ezetimibe to Statin Therapy in Heart Transplants Recipients at High Risk of Cardiac Allograft Progression: A Multicenter Target Trial EmulationHsieh Rebecca, Kumar Agara, Lee Pei-lun, Chi Kuan Yu, Tran Viet Nghi, Wang Yu-chiang