Final ID: MP510
Reducing Carbohydrate Quantity Lowers 10-Year Predicted Risk of Cardiovascular Disease Using the PREVENT Equation: An Ancillary Study of the OMNICARB Trial
Abstract Body (Do not enter title and authors here): Background
Cardiovascular disease (CVD) remains a leading cause of death in the United States. While evidence suggests that lowering carbohydrate quantity may improve CVD risk factors and the effects of lowering carbohydrate quality [glycemic index (GI)] are mixed, their effects on predicted CVD risk remain unexplored. The American Heart Association's Predicting Risk of CVD EVENTs (PREVENT) equations offer a modern approach to CVD risk prediction. However, their application in dietary interventions targeting macronutrients is yet to be explored.
Hypothesis
Evaluate the impact of dietary carbohydrate quantity and GI on 10-year predicted CVD risk using PREVENT. We hypothesized that a low-carbohydrate, low-GI diet would reduce 10-year predicted CVD risk.
Methods
OmniCarb (NCT00608049), a 4-period randomized crossover feeding study, examined the effects of dietary GI on CVD risk factors. Overweight/obese adults without CVD were randomized to 1 of 8 diet sequences, receiving 4 isocaloric, healthful DASH-type diets (cg, cG, Cg, and CG; see Figure 1 for definitions) for 5 weeks each, with 2-week washouts. Predicted 10-year CVD risk was estimated using the base PREVENT model at baseline and after each diet period. Linear mixed-effects models assessed within-person differences in predicted risk across diets. Primary outcomes were absolute and relative differences in predicted CVD risk from baseline.
Results
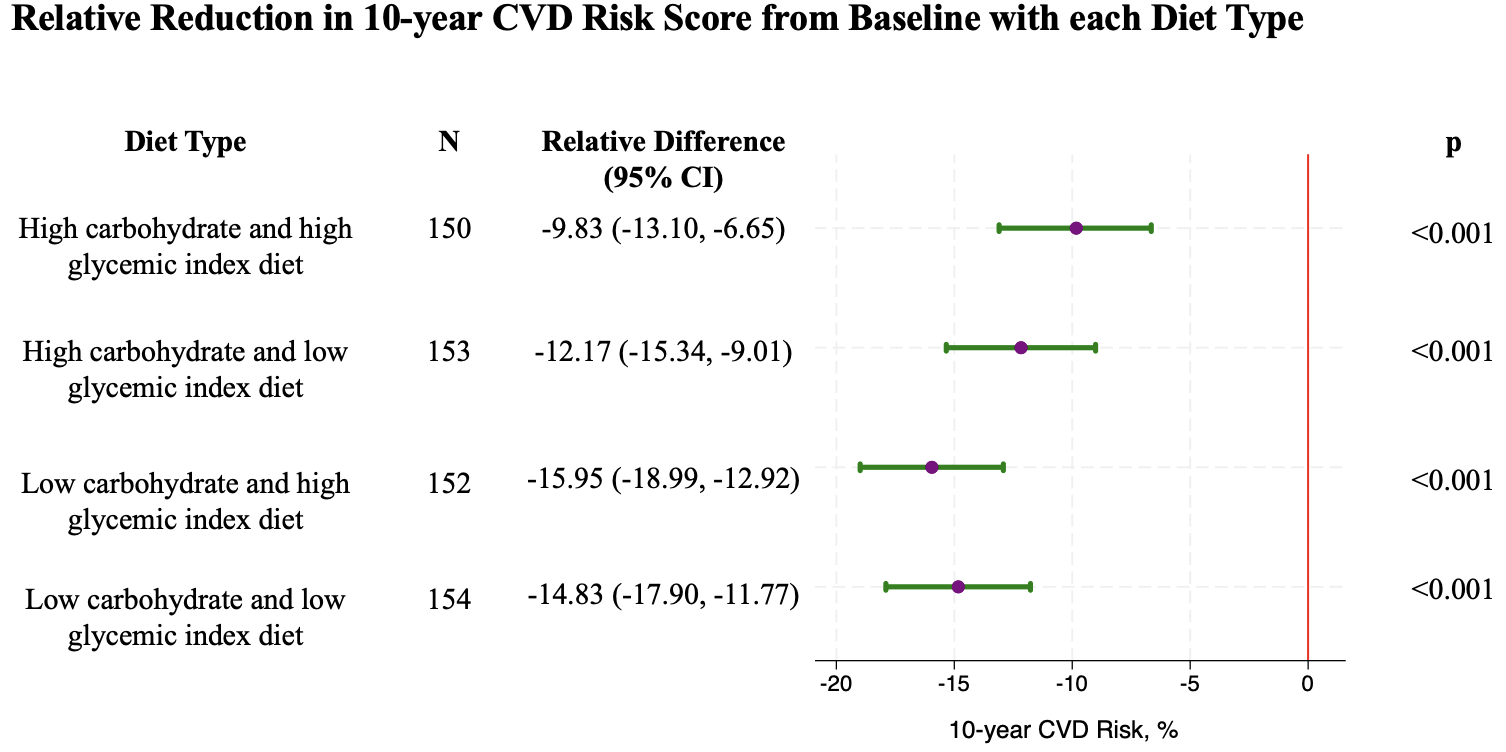
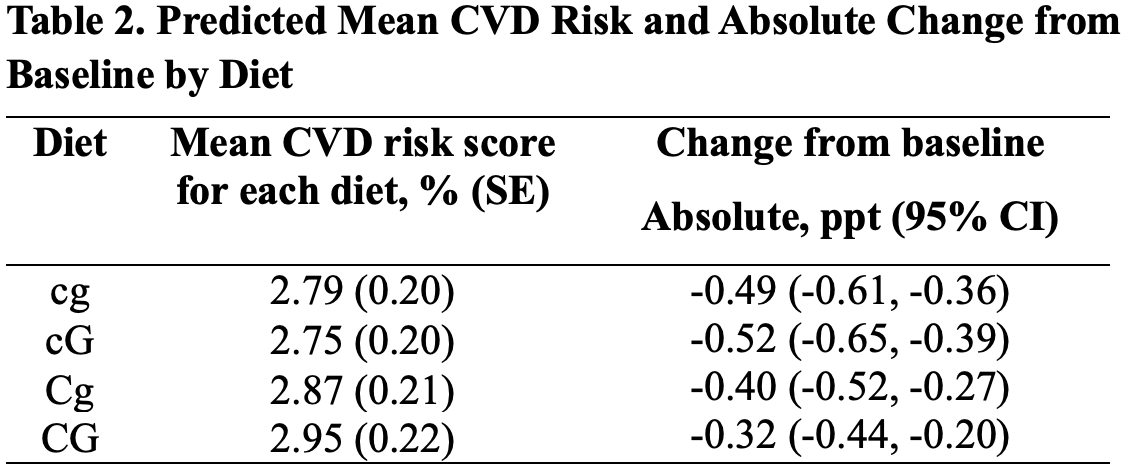
Among 163 participants (mean [SD] age 52 [11] years; 52% female; 51% Black/African American, 56% obese, 64% never smokers) who completed at least 2 diet periods, median (IQR) baseline predicted risk was 3.8% (1.7%-6.0%); mean (SD) was 4.6% (3.9%). All intervention diets showed modest reductions in absolute predicted risk from baseline (Table 2). Relative reductions compared to baseline were greatest for cG and cg (Figure 1). Compared to cg, CG was associated with significantly higher predicted CVD risk (p = 0.002), while differences for cG (p = 0.493) and Cg (p = 0.092) were not significant. Compared to low-carbohydrate diets, high-carbohydrate diets were associated with a higher predicted risk (p < 0.001), whereas high-GI diets had no significant difference in risk compared to the low-GI diets (p = 0.598).
Conclusion
Reducing carbohydrate quantity, regardless of GI, led to the greatest reductions in 10-year predicted CVD risk, suggesting that carbohydrate content may be a more effective dietary target than GI for lowering cardiovascular risk in at-risk adults.
Cardiovascular disease (CVD) remains a leading cause of death in the United States. While evidence suggests that lowering carbohydrate quantity may improve CVD risk factors and the effects of lowering carbohydrate quality [glycemic index (GI)] are mixed, their effects on predicted CVD risk remain unexplored. The American Heart Association's Predicting Risk of CVD EVENTs (PREVENT) equations offer a modern approach to CVD risk prediction. However, their application in dietary interventions targeting macronutrients is yet to be explored.
Hypothesis
Evaluate the impact of dietary carbohydrate quantity and GI on 10-year predicted CVD risk using PREVENT. We hypothesized that a low-carbohydrate, low-GI diet would reduce 10-year predicted CVD risk.
Methods
OmniCarb (NCT00608049), a 4-period randomized crossover feeding study, examined the effects of dietary GI on CVD risk factors. Overweight/obese adults without CVD were randomized to 1 of 8 diet sequences, receiving 4 isocaloric, healthful DASH-type diets (cg, cG, Cg, and CG; see Figure 1 for definitions) for 5 weeks each, with 2-week washouts. Predicted 10-year CVD risk was estimated using the base PREVENT model at baseline and after each diet period. Linear mixed-effects models assessed within-person differences in predicted risk across diets. Primary outcomes were absolute and relative differences in predicted CVD risk from baseline.
Results
Among 163 participants (mean [SD] age 52 [11] years; 52% female; 51% Black/African American, 56% obese, 64% never smokers) who completed at least 2 diet periods, median (IQR) baseline predicted risk was 3.8% (1.7%-6.0%); mean (SD) was 4.6% (3.9%). All intervention diets showed modest reductions in absolute predicted risk from baseline (Table 2). Relative reductions compared to baseline were greatest for cG and cg (Figure 1). Compared to cg, CG was associated with significantly higher predicted CVD risk (p = 0.002), while differences for cG (p = 0.493) and Cg (p = 0.092) were not significant. Compared to low-carbohydrate diets, high-carbohydrate diets were associated with a higher predicted risk (p < 0.001), whereas high-GI diets had no significant difference in risk compared to the low-GI diets (p = 0.598).
Conclusion
Reducing carbohydrate quantity, regardless of GI, led to the greatest reductions in 10-year predicted CVD risk, suggesting that carbohydrate content may be a more effective dietary target than GI for lowering cardiovascular risk in at-risk adults.
More abstracts on this topic:
A Model-Sharing Approach for Quality Improvement of Diabetes and Cardiovascular Disease
Elligers Kyle, Pollner Meghan, Overton Katherine, Congdon Michelle, Greenway Stacey, Lambro Patricia, Sadiku Steven, Schechter Rona, Whelan John, Pressley Bianca, Sednew Renee, Duckett Sara
A validated metabolite-based biomarker score for fruit and vegetable intake and associations with all-cause mortality and incident cardiometabolic diseasesOude Griep Linda, Li Chunxiao, Koulman Albert, Imamura Fumiaki, Wareham Nicholas, Forouhi Nita