Final ID: MP2690
Survival Benefit of Beta-Adrenergic Suppression Following Lung Transplantation
Abstract Body (Do not enter title and authors here): Introduction
Long-term survival following lung transplant surgery (LT) presents an ongoing challenge, with a five-year survival rate of 55%. Furthermore, adverse LT outcomes are linked to a high incidence of cardiac arrhythmias. Although beta-adrenergic suppression (BAS) can be safely initiated in most patients with severe lung disease, current guideline documents indicate that the role of BAS after LT remains unclear. Therefore, the safety and potential benefits of BAS on long-term survival after LT remain to be determined.
Methods
All adult patients who underwent LT at the University of Florida between 2016 and 2021 were identified. Their pre- and post-LT medication use, as well as relevant patient characteristics, comorbidities, and follow-up data (including survival), were recorded in a dedicated database.
Results
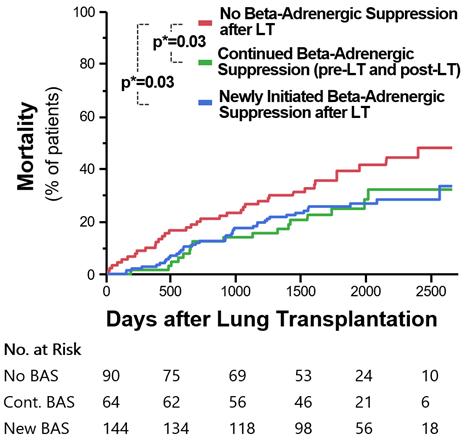
The LT recipients included in this study (N=299) had mean age 60 ± 11 years, 45% were female, mean body mass index was 26 ± 6kg/m2. Available mean follow up was 4.5 ± 1.9 years. BAS medications were used by 85 (28%) patients pre-LT, and by 210 (70%) patients after LT. A significant survival benefit was evident in patients who were already receiving BAS prior to LT and continued its use post-LT (p = 0.03). Those newly initiated on BAS after LT manifested a comparable survival benefit relative to patients not receiving BAS (p = 0.03, Figure). A combined analysis revealed that all patients for whom BAS was prescribed after LT exhibited prolonged survival when compared to patients without BAS (p = 0.008, adjusted in a multivariate analysis for age, sex, history of smoking, renal insufficiency, coronary artery
disease, heart failure, hypertension, hyperlipidemia, and sleep apnea). No survival benefit was observed when analyzing other classes of anti-arrhythmic drugs including Amiodarone after LT.
Conclusions
In this large, retrospective, single-center study of long-term survival after LT, patients using BAS lived significantly longer, even after accounting for potential confounders. This benefit extended to both patients newly initiated on BAS and those who were using BAS pre-LT and continued it post-LT. Consequently, routine use of BAS should be considered in appropriate LT patients. Future studies are warranted to build upon these findings, particularly to identify and maximize the potential protective pathophysiologic mechanisms.
Long-term survival following lung transplant surgery (LT) presents an ongoing challenge, with a five-year survival rate of 55%. Furthermore, adverse LT outcomes are linked to a high incidence of cardiac arrhythmias. Although beta-adrenergic suppression (BAS) can be safely initiated in most patients with severe lung disease, current guideline documents indicate that the role of BAS after LT remains unclear. Therefore, the safety and potential benefits of BAS on long-term survival after LT remain to be determined.
Methods
All adult patients who underwent LT at the University of Florida between 2016 and 2021 were identified. Their pre- and post-LT medication use, as well as relevant patient characteristics, comorbidities, and follow-up data (including survival), were recorded in a dedicated database.
Results
The LT recipients included in this study (N=299) had mean age 60 ± 11 years, 45% were female, mean body mass index was 26 ± 6kg/m2. Available mean follow up was 4.5 ± 1.9 years. BAS medications were used by 85 (28%) patients pre-LT, and by 210 (70%) patients after LT. A significant survival benefit was evident in patients who were already receiving BAS prior to LT and continued its use post-LT (p = 0.03). Those newly initiated on BAS after LT manifested a comparable survival benefit relative to patients not receiving BAS (p = 0.03, Figure). A combined analysis revealed that all patients for whom BAS was prescribed after LT exhibited prolonged survival when compared to patients without BAS (p = 0.008, adjusted in a multivariate analysis for age, sex, history of smoking, renal insufficiency, coronary artery
disease, heart failure, hypertension, hyperlipidemia, and sleep apnea). No survival benefit was observed when analyzing other classes of anti-arrhythmic drugs including Amiodarone after LT.
Conclusions
In this large, retrospective, single-center study of long-term survival after LT, patients using BAS lived significantly longer, even after accounting for potential confounders. This benefit extended to both patients newly initiated on BAS and those who were using BAS pre-LT and continued it post-LT. Consequently, routine use of BAS should be considered in appropriate LT patients. Future studies are warranted to build upon these findings, particularly to identify and maximize the potential protective pathophysiologic mechanisms.
More abstracts on this topic:
A Heart-pounding Case of Cardiomyopathy in Pregnancy
Tran Linh, Everitt Ian, Vaught Arthur, Barth Andreas, Minhas Anum
Allograft Outcomes of Adding Proprotein Convertase Subtilisin Kexin 9 Inhibitors or Ezetimibe to Statin Therapy in Heart Transplants Recipients at High Risk of Cardiac Allograft Progression: A Multicenter Target Trial EmulationHsieh Rebecca, Kumar Agara, Lee Pei-lun, Chi Kuan Yu, Tran Viet Nghi, Wang Yu-chiang