Final ID: MP2520
Transforming Heart Failure Care with EHR-Based Alerts: Accurate Diagnosis and Improved GDMT Uptake
Abstract Body (Do not enter title and authors here): Introduction/Background
Guideline-directed medical therapy (GDMT) is central to managing heart failure (HF) with reduced ejection fraction (HFrEF), offering up to a 73% reduction in mortality. National guidelines assign GDMT a Class I recommendation. However, accurately identifying HFrEF patients remains a challenge, as International Classification of Disease codes and claims data are inaccurate up to 25%. At our academic institution, “HF unspecified” was the most frequently documented diagnosis, limiting targeted interventions and quality care assessment. To address this gap, we developed an electronic health record (EHR) integrated Best Practice Advisory (BPA) to accurately classify patients, support a system-wide HF registry and underpin a quality incentive program.
Research Questions/Hypothesis
We hypothesized that implementing a BPA would improve classification accuracy into HFrEF, HFmrEF, or HFpEF; identify HF patients previously missed by documentation gaps; and increase GDMT adherence.
Methods/Approach
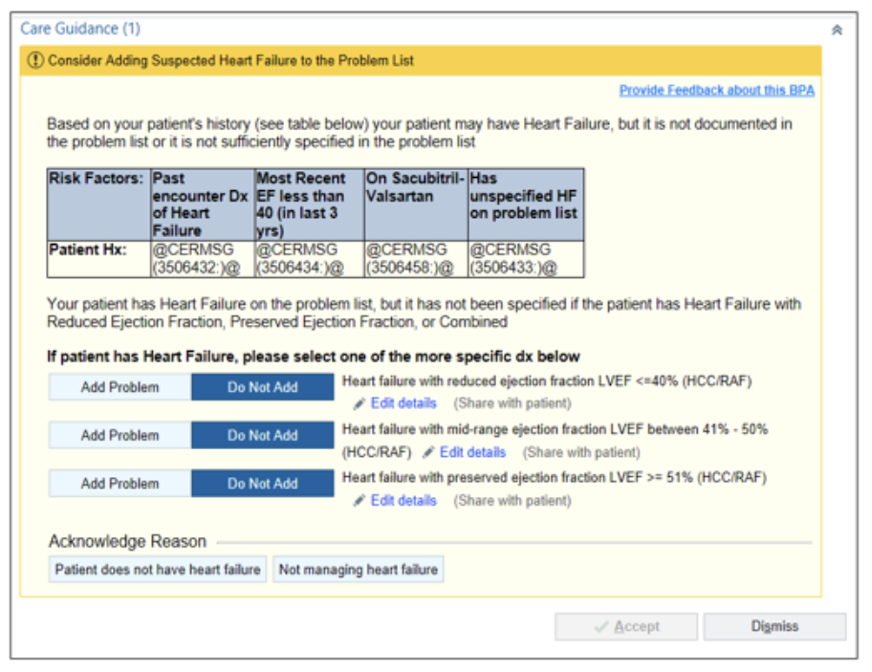
A BPA was created to trigger during primary care and cardiology encounters for patients meeting criteria suggestive of HFrEF (e.g., ejection fraction (EF) ≤40%, nonspecific HF diagnosis, repeated HF billing, sacubitril-valsartan use, or high-risk comorbidities). Exclusion criteria included hospice, transplant, LVAD, pregnancy, or breastfeeding. The BPA was piloted across 15 clinics, refined through provider feedback, and integrated into a system-wide HF registry. It was also linked to a financial incentive program rewarding GDMT performance in HFrEF patients.
Results/Data (descriptive and inferential statistics)
Over 42 months, the BPA identified and reclassified 10,920 patients (up from 7,081). The “HF unspecified” diagnosis declined from 2,483 to 1,465 patients (35% to 13%). Concurrently, HFrEF diagnoses increased from 2,832 to 4,518, HFmrEF from 29 to 700, and HFpEF from 2,176 to 4,707. Total HF patient identification rose by 150%, reflecting improved documentation and accurate capture of previously missed cases.
Conclusion
An EHR-integrated BPA significantly improved HF identification and reclassification, reduced nonspecific coding, enabled registry development, and supported a scalable quality initiative. This intervention enabled targeted GDMT optimization and offers a replicable model for chronic disease population health management.
Guideline-directed medical therapy (GDMT) is central to managing heart failure (HF) with reduced ejection fraction (HFrEF), offering up to a 73% reduction in mortality. National guidelines assign GDMT a Class I recommendation. However, accurately identifying HFrEF patients remains a challenge, as International Classification of Disease codes and claims data are inaccurate up to 25%. At our academic institution, “HF unspecified” was the most frequently documented diagnosis, limiting targeted interventions and quality care assessment. To address this gap, we developed an electronic health record (EHR) integrated Best Practice Advisory (BPA) to accurately classify patients, support a system-wide HF registry and underpin a quality incentive program.
Research Questions/Hypothesis
We hypothesized that implementing a BPA would improve classification accuracy into HFrEF, HFmrEF, or HFpEF; identify HF patients previously missed by documentation gaps; and increase GDMT adherence.
Methods/Approach
A BPA was created to trigger during primary care and cardiology encounters for patients meeting criteria suggestive of HFrEF (e.g., ejection fraction (EF) ≤40%, nonspecific HF diagnosis, repeated HF billing, sacubitril-valsartan use, or high-risk comorbidities). Exclusion criteria included hospice, transplant, LVAD, pregnancy, or breastfeeding. The BPA was piloted across 15 clinics, refined through provider feedback, and integrated into a system-wide HF registry. It was also linked to a financial incentive program rewarding GDMT performance in HFrEF patients.
Results/Data (descriptive and inferential statistics)
Over 42 months, the BPA identified and reclassified 10,920 patients (up from 7,081). The “HF unspecified” diagnosis declined from 2,483 to 1,465 patients (35% to 13%). Concurrently, HFrEF diagnoses increased from 2,832 to 4,518, HFmrEF from 29 to 700, and HFpEF from 2,176 to 4,707. Total HF patient identification rose by 150%, reflecting improved documentation and accurate capture of previously missed cases.
Conclusion
An EHR-integrated BPA significantly improved HF identification and reclassification, reduced nonspecific coding, enabled registry development, and supported a scalable quality initiative. This intervention enabled targeted GDMT optimization and offers a replicable model for chronic disease population health management.
More abstracts on this topic:
A Novel Approach to Manage Hypercholesterolemia: The Veterans Affairs Lipid Optimization Reimagined Quality Improvement (VALOR-QI) Program
Djousse Luc, Leesch Tharen, Pena David, Gaziano Michael, Ward Rachel, Wellman Helen, Yel Nedim, Santos Abigail, Delgrande Jen, Fink Abigail, Colson Kristin, Pan Eddie
A Case of Dilated Cardiomyopathy and Systemic Thromboembolism in a Young Patient on Testosterone Replacement TherapySabri Muhammad, Ijaz Naila, Nadeem Ramsha, Checchio Lucy, Riaz Faiza