Final ID: MP2649
Pulse Field Ablation Have A Mild Impact on Atrial Fibrillation Ablation Workflow And Organization: A Single High-Volume Center Experience
Abstract Body (Do not enter title and authors here): INTRODUCTION AND BACKGROUND
Pulsed field ablation (PFA) is a new non-thermal energy source with a selective effect on myocardial cells that limits damage to other tissues. Because it is more painful, it needs to be performed under general anesthesia or deep sedation.
RESEARCH QUESTIONS
We would assess if PFA compared to radiofrequency ablation (RFA) could have an impact on procedural organization and workflow of atrial fibrillation (AF) ablation, including effects on vagal nervous system.
METHODS
In this retrospective case-control study we analyzed paroxysmal or persistent AF ablations by pulmonary vein isolation, performed over the last year, 2024, in our high-volume center. The population was divided into two matched samples: PFA group under deep sedation and RFA under light sedation. All procedures were supported by electro-anatomical mapping. We collected all procedural times as primary outcome, then we examined all other procedural data and vagal ganglionated plexi (GPs) involvement.
RESULTS AND DATA
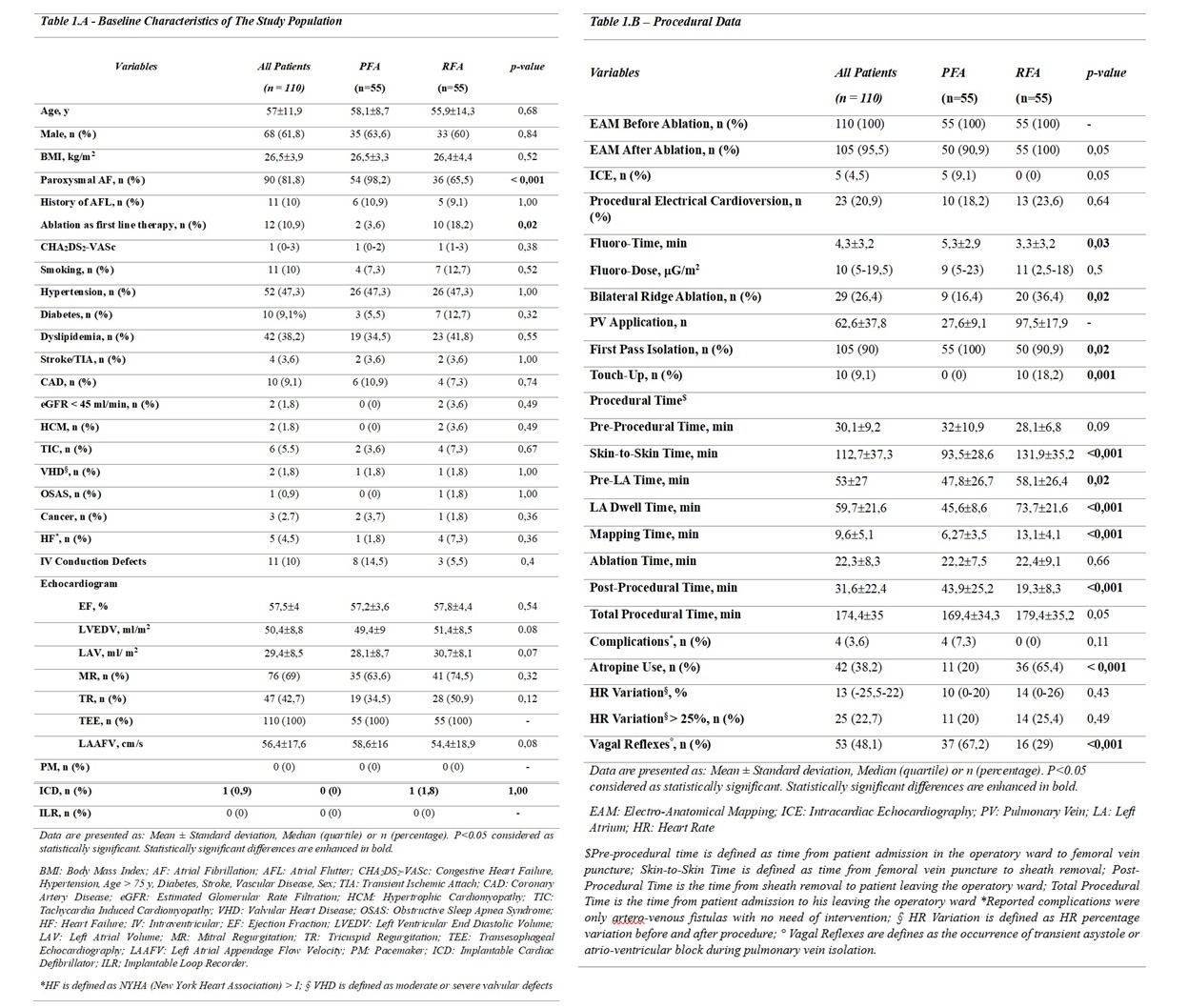
This study included 110 Caucasian patients (mean age 57±11,9, 61,8% males), 55 in PFA (mean age 58,1±8,7, 63,6% males) and 55 RFA group (mean age 55,9±14,3, 60% males). Baseline characteristics of patients are reported in fig.1.
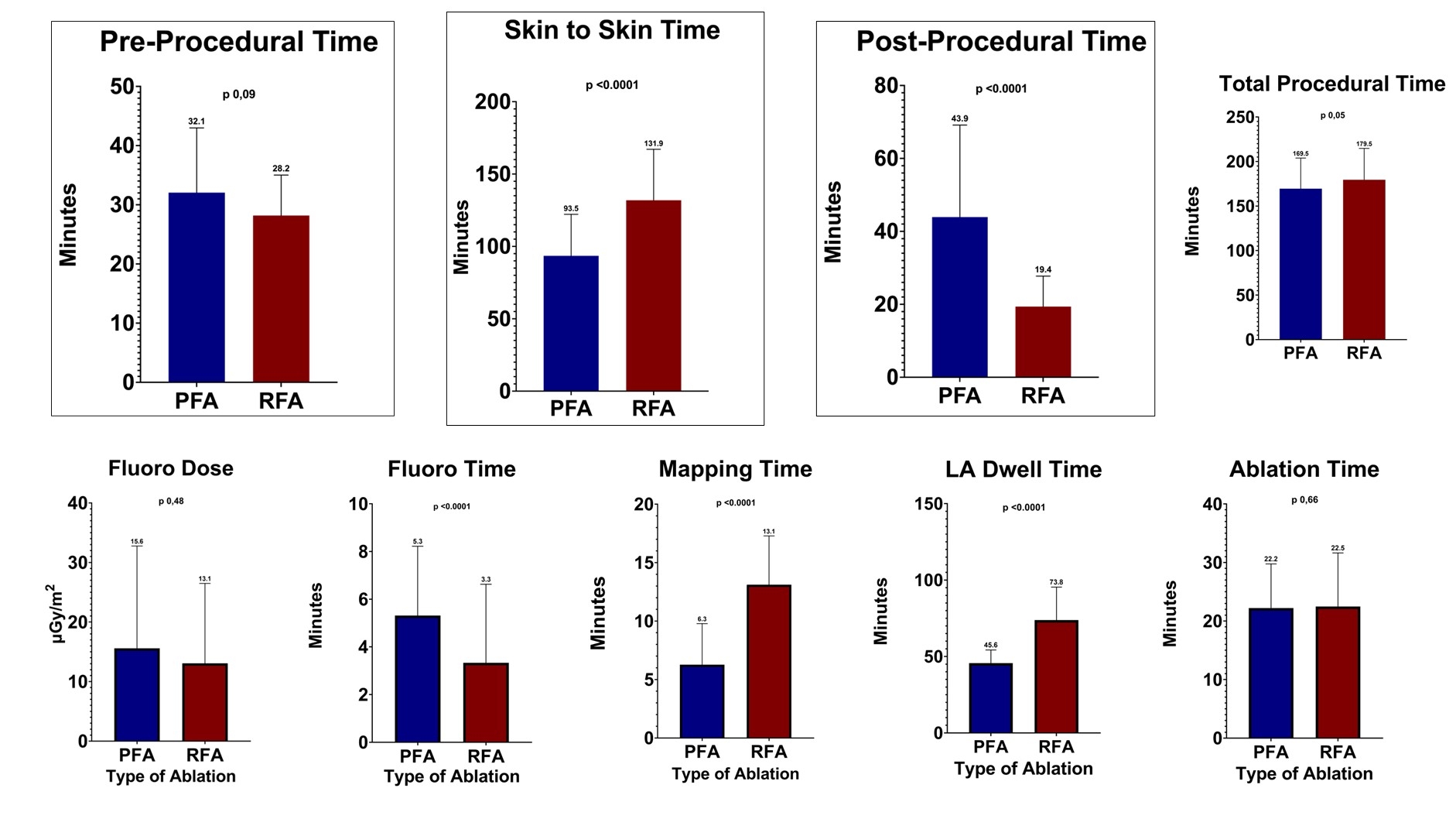
Longer post-procedural time (43,9±25,2 vs 19,3±8,3 min; p <0,001) was reported in PFA group. On the contrary, shorter skin to skin times (93,5±28,6 vs 131,9±35,2 min; p <0,001), mapping times (6,27±3,5 vs 13,1±4,1 min; p <0,001) and left atrium dwell times (45,6±8,6 vs 73,7±21,6 min; p <0,001) were evidenced for electroporation. No statistical differences were documented between PFA and RFA about pre-procedural (32±10,9 vs 28,1±6,8 min; p 0,96), ablation (22,2±7,5 vs 22,4±9,1 min; p 0,66) and total procedural times (169,47±34,3 vs 179,4±35,2 min; p 0,05). Interestingly, fluoro-time was shorter in RFA (5,3±2,9 vs 3,3±3,2 min; p <0,001), but fluoro-dose was similar (15,3±17,2 vs 13±13,4 mGy/m2; p 0,56). Complication rate was very low for both.
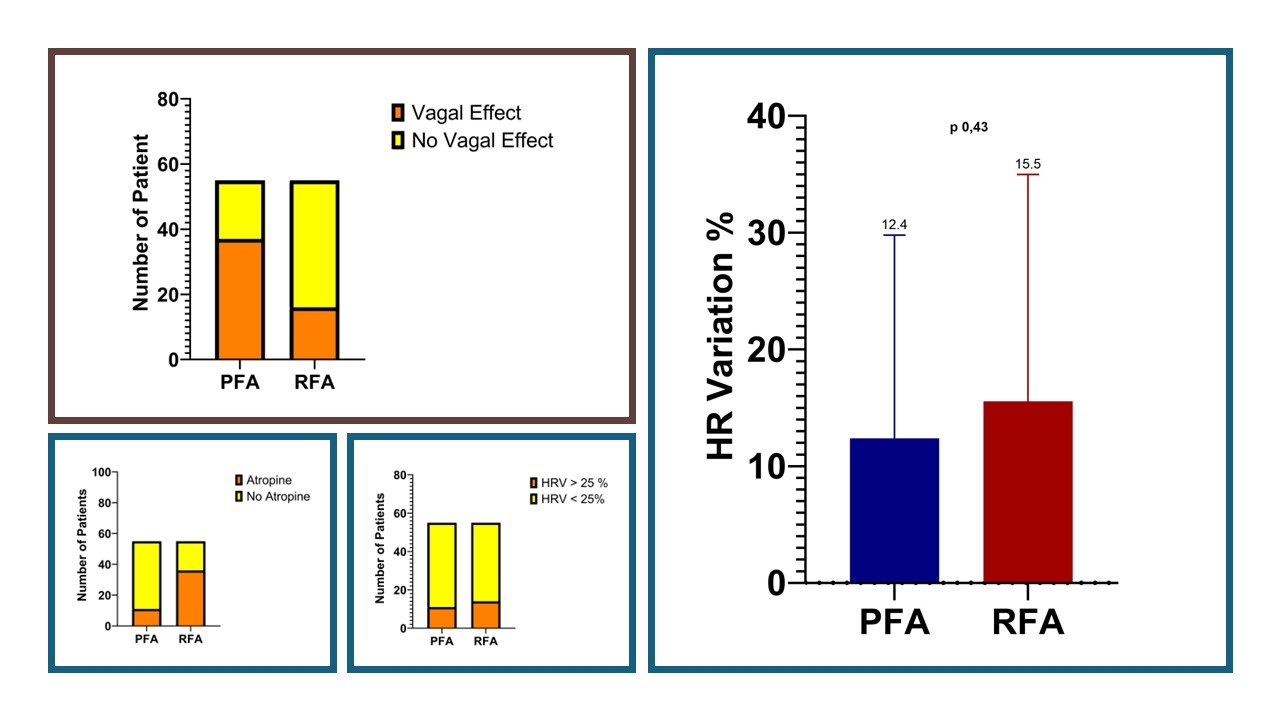
About GPs involvement, heart rate variation before and after procedure was similar between PFA and RFA (fig.1). Interstingly, vagal reflexes were more frequently induced using PFA (67,2% vs 30,1%; p <0,001) and atropine use was more in RFA group (20% vs 65,4%; p <0,001).
CONCLUSIONS
PFA is efficient, safe and feasible with mild impact on periprocedural workflow and organization of AF ablation using deep sedation. Vagal effects were often induced by PFA without clinical effects as compared to RFA.
Pulsed field ablation (PFA) is a new non-thermal energy source with a selective effect on myocardial cells that limits damage to other tissues. Because it is more painful, it needs to be performed under general anesthesia or deep sedation.
RESEARCH QUESTIONS
We would assess if PFA compared to radiofrequency ablation (RFA) could have an impact on procedural organization and workflow of atrial fibrillation (AF) ablation, including effects on vagal nervous system.
METHODS
In this retrospective case-control study we analyzed paroxysmal or persistent AF ablations by pulmonary vein isolation, performed over the last year, 2024, in our high-volume center. The population was divided into two matched samples: PFA group under deep sedation and RFA under light sedation. All procedures were supported by electro-anatomical mapping. We collected all procedural times as primary outcome, then we examined all other procedural data and vagal ganglionated plexi (GPs) involvement.
RESULTS AND DATA
This study included 110 Caucasian patients (mean age 57±11,9, 61,8% males), 55 in PFA (mean age 58,1±8,7, 63,6% males) and 55 RFA group (mean age 55,9±14,3, 60% males). Baseline characteristics of patients are reported in fig.1.
Longer post-procedural time (43,9±25,2 vs 19,3±8,3 min; p <0,001) was reported in PFA group. On the contrary, shorter skin to skin times (93,5±28,6 vs 131,9±35,2 min; p <0,001), mapping times (6,27±3,5 vs 13,1±4,1 min; p <0,001) and left atrium dwell times (45,6±8,6 vs 73,7±21,6 min; p <0,001) were evidenced for electroporation. No statistical differences were documented between PFA and RFA about pre-procedural (32±10,9 vs 28,1±6,8 min; p 0,96), ablation (22,2±7,5 vs 22,4±9,1 min; p 0,66) and total procedural times (169,47±34,3 vs 179,4±35,2 min; p 0,05). Interestingly, fluoro-time was shorter in RFA (5,3±2,9 vs 3,3±3,2 min; p <0,001), but fluoro-dose was similar (15,3±17,2 vs 13±13,4 mGy/m2; p 0,56). Complication rate was very low for both.
About GPs involvement, heart rate variation before and after procedure was similar between PFA and RFA (fig.1). Interstingly, vagal reflexes were more frequently induced using PFA (67,2% vs 30,1%; p <0,001) and atropine use was more in RFA group (20% vs 65,4%; p <0,001).
CONCLUSIONS
PFA is efficient, safe and feasible with mild impact on periprocedural workflow and organization of AF ablation using deep sedation. Vagal effects were often induced by PFA without clinical effects as compared to RFA.
More abstracts on this topic:
4D Cardiac Optogenetics Enable Complex Arrhythmia Modelling and Precise Interventional Simulation
Wexler Yehuda, Grinstein Harel, Landesberg Michal, Glatstein Shany, Huber Irit, Arbel Gil, Gepstein Lior
4D Cardiac Optogenetics Enable Complex Arrhythmia Modelling and Precise Interventional SimulationWexler Yehuda, Grinstein Harel, Landesberg Michal, Glatstein Shany, Huber Irit, Arbel Gil, Gepstein Lior