Final ID: MP1472
Intervention to Increase Screening and Treatment of Iron Deficiency in Heart Failure Patients in the Acute Care Setting
Abstract Body (Do not enter title and authors here): Patients with heart failure with reduced ejection fraction are at high risk for iron deficiency (ID) due to low intake and high losses. Randomized controlled trials show intravenous (IV) iron improves quality of life and lowers readmissions. Suboptimal ID screening may stem from limited awareness of ID thresholds and guidelines in heart failure. We hypothesized that implementing provider education and optimized EHR notification would improve ID screening and IV iron infusion rates over 6 months among inpatients at a community hospital.
Presentations were delivered to the Internal Medicine Residents, Hospitalists, and Cardiologists, reviewing key trials and recommendations for ID in CHF from the European Society of Cardiology (ESC), the American College of Cardiology (ACC), and the American Heart Association (AHA). A flyer summarizing diagnostic criteria and IV iron treatment was then posted in high-traffic provider areas. A Best Practice Alert (BPA) was also implemented, which triggered if a patient had heart failure and no iron studies in the past 6 months, automatically adding iron study orders unless removed. IV iron was recommended through education via presentations and flyers, using criteria of ferritin <100 ng/mL or 100–299 ng/mL with TSAT <20%.
Pre-intervention data (PRE) were collected from 10/1/2024 - 2/13/2025, and post-intervention (POST) from 2/14 - 5/20/2025. Exclusions included previous iron studies or iron supplementation within 6 months. A chi-square test of independence was performed to measure if there was a statistically significant difference between PRE and POST for ID screening, IV infusion, and oral iron rates.
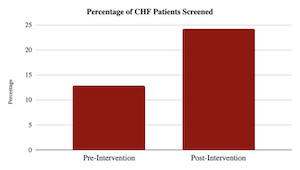
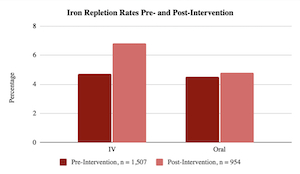
2,461 encounters met inclusion criteria (PRE: 1,507, POST: 954). Prior to the intervention, 12.8% were screened for ID compared to 24.1% after intervention with an Absolute Benefit Increase of 11.3% (p < 0.001). The rate of IV iron repletion increased significantly (PRE: 4.8% vs. POST: 6.8%, p < 0.05). Oral iron repletion rates were not significantly different in PRE vs. POST (4.5% to 4.8%, p > 0.05).
ID screening improved with minimal burden via provider education and BPAs. IV iron use rose modestly, limited by reliance on education alone and brief hospital stays with competing clinical priorities. Future efforts should target education on oral iron absorption limitations, investigate barriers to IV iron infusion, and optimize the outpatient transition for continued ID management.
Presentations were delivered to the Internal Medicine Residents, Hospitalists, and Cardiologists, reviewing key trials and recommendations for ID in CHF from the European Society of Cardiology (ESC), the American College of Cardiology (ACC), and the American Heart Association (AHA). A flyer summarizing diagnostic criteria and IV iron treatment was then posted in high-traffic provider areas. A Best Practice Alert (BPA) was also implemented, which triggered if a patient had heart failure and no iron studies in the past 6 months, automatically adding iron study orders unless removed. IV iron was recommended through education via presentations and flyers, using criteria of ferritin <100 ng/mL or 100–299 ng/mL with TSAT <20%.
Pre-intervention data (PRE) were collected from 10/1/2024 - 2/13/2025, and post-intervention (POST) from 2/14 - 5/20/2025. Exclusions included previous iron studies or iron supplementation within 6 months. A chi-square test of independence was performed to measure if there was a statistically significant difference between PRE and POST for ID screening, IV infusion, and oral iron rates.
2,461 encounters met inclusion criteria (PRE: 1,507, POST: 954). Prior to the intervention, 12.8% were screened for ID compared to 24.1% after intervention with an Absolute Benefit Increase of 11.3% (p < 0.001). The rate of IV iron repletion increased significantly (PRE: 4.8% vs. POST: 6.8%, p < 0.05). Oral iron repletion rates were not significantly different in PRE vs. POST (4.5% to 4.8%, p > 0.05).
ID screening improved with minimal burden via provider education and BPAs. IV iron use rose modestly, limited by reliance on education alone and brief hospital stays with competing clinical priorities. Future efforts should target education on oral iron absorption limitations, investigate barriers to IV iron infusion, and optimize the outpatient transition for continued ID management.
More abstracts on this topic:
Cardiac Arrhythmia-Related Mortality in Adults with Aplastic Anemia in the United States: A 25-Year Nationwide Analysis (1999–2023)
Ahmad Husnain, Patel Palak, Ali Muhammad Faizan, Oza Jaykumar, Rahim Muhammad
Blood Volume Prediction Equations Do Not Precisely Estimate Blood Volume in Adults with Heart Failure with Preserved Ejection Fraction (HFpEF)Sooda Meera, Levine Benjamin, Wakeham Denis, Samels Mitchel, Brazile Tiffany, Leahy Michael, Manferdelli Giorgio, Macnamara James, Sarma Satyam, Hearon Christopher