Final ID: MP129
Clinical and Echocardiographic Predictors of Aortopathy in Patients with Bicuspid Aortic Valve: Insights from a Large Community Cohort
Abstract Body (Do not enter title and authors here): Background
The bicuspid aortic valve (BAV) is the most prevalent congenital heart defect and is frequently associated with aortopathy. The etiology of aortic dilation in BAV is multifactorial, involving both hemodynamic stress and intrinsic aortic wall abnormalities. While previous studies have proposed several mechanisms, the specific and valve-related predictors of aortopathy remain unclear.
Research question
Which clinical and echocardiographic features independently predict the presence of aortopathy in patients with BAV?
Goals
To identify the patient and value-related characteristics associated with aortopathy in a large, real-world BAV cohort using standardized imaging and statistical approaches.
Approach
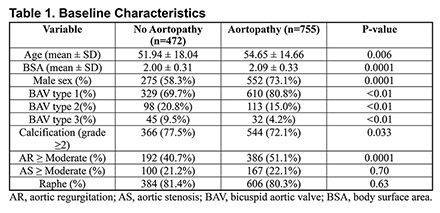
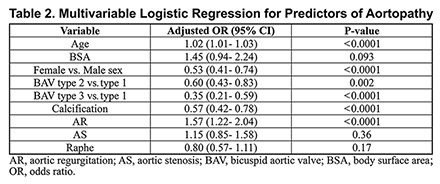
Between 2013 and 2017, across 33 echocardiography labs within a large U.S. health system, 1,227 patients diagnosed with BAV were retrospectively reviewed. BAV morphology, presence of raphe, calcification severity (grades 0-4), aortic regurgitation (AR), aortic stenosis (AS), age, sex, and body surface area (BSA) were collected. Aortopathy was defined based on measurements of the aorta at the sinus of Valsalva and mid-ascending portions, indexed to body surface area. Univariate analysis (Mann-Whitney U and Chi-square) identified candidate predictors. A multivariable logistic regression model was constructed to identify independent predictors of aortopathy. Multicollinearity was assessed using the variance inflation factor and tolerance.
Results
Among 1,227 BAV patients, 755 (61.5%) had aortopathy. They were older (54.7 vs. 51.9 years, p=0.006), had higher BSA (2.09 vs. 2.00 m2, p<0.001), and were more often male (73.1% vs. 58.3%, p<0.001). Independent predictors of aortopathy included male sex, age, AR severity, and BAV Type 1 (vs. Types 2 and 3). Calcification was inversely associated. AS, BSA, and raphe were not significant predictors. The model demonstrated excellent calibration (Hosmer-Lemeshow p = 0.715).
Conclusion
Clinical characteristics emerge to differentiate BAV patients with aortopathy. Although the relationships between aortopathy and BAV are complex, specific clinical and echocardiographic variables in this cohort, particularly BAV Type 1, age, Male sex, calcification, and AR severity, were independently associated with aortopathy. These findings support multifactorial pathogenesis of BAV-associated aortopathy and may inform future risk stratification and surveillance strategies.
The bicuspid aortic valve (BAV) is the most prevalent congenital heart defect and is frequently associated with aortopathy. The etiology of aortic dilation in BAV is multifactorial, involving both hemodynamic stress and intrinsic aortic wall abnormalities. While previous studies have proposed several mechanisms, the specific and valve-related predictors of aortopathy remain unclear.
Research question
Which clinical and echocardiographic features independently predict the presence of aortopathy in patients with BAV?
Goals
To identify the patient and value-related characteristics associated with aortopathy in a large, real-world BAV cohort using standardized imaging and statistical approaches.
Approach
Between 2013 and 2017, across 33 echocardiography labs within a large U.S. health system, 1,227 patients diagnosed with BAV were retrospectively reviewed. BAV morphology, presence of raphe, calcification severity (grades 0-4), aortic regurgitation (AR), aortic stenosis (AS), age, sex, and body surface area (BSA) were collected. Aortopathy was defined based on measurements of the aorta at the sinus of Valsalva and mid-ascending portions, indexed to body surface area. Univariate analysis (Mann-Whitney U and Chi-square) identified candidate predictors. A multivariable logistic regression model was constructed to identify independent predictors of aortopathy. Multicollinearity was assessed using the variance inflation factor and tolerance.
Results
Among 1,227 BAV patients, 755 (61.5%) had aortopathy. They were older (54.7 vs. 51.9 years, p=0.006), had higher BSA (2.09 vs. 2.00 m2, p<0.001), and were more often male (73.1% vs. 58.3%, p<0.001). Independent predictors of aortopathy included male sex, age, AR severity, and BAV Type 1 (vs. Types 2 and 3). Calcification was inversely associated. AS, BSA, and raphe were not significant predictors. The model demonstrated excellent calibration (Hosmer-Lemeshow p = 0.715).
Conclusion
Clinical characteristics emerge to differentiate BAV patients with aortopathy. Although the relationships between aortopathy and BAV are complex, specific clinical and echocardiographic variables in this cohort, particularly BAV Type 1, age, Male sex, calcification, and AR severity, were independently associated with aortopathy. These findings support multifactorial pathogenesis of BAV-associated aortopathy and may inform future risk stratification and surveillance strategies.
More abstracts on this topic:
A Novel Echocardiography Risk Score Predicted Mortality In Patients With Heart Failure With Preserved Ejection Fraction.
Iwakura Katsuomi, Yoshio Yasumura, Hikoso Shungo, Okada Katsuki, Nakatani Daisaku, Sotomi Yohei, Sakata Yasushi, Tanaka Nobuaki, Okada Masato, Okamura Atsunori, Heitaro Watanabe, Seo Masahiro, Hayashi Takaharu, Yano Masamichi, Yamada Takahisa
A drug target Mendelian randomization study of triglyceride lowering therapies for aortic stenosisCiofani Jonathan, Han Daniel, Gill Dipender, Rao Karan, Allahwala Usaid, Bhindi Ravinay