Final ID: Su4012
Genetic determinants of left ventricular diastolic function
Abstract Body (Do not enter title and authors here): Background
Left ventricular (LV) diastolic function relies on active myocardial relaxation and passive cardiac chamber stiffness and is assessed by echocardiography. Abnormal LV diastolic function portends worse outcomes in heart failure (HF), cardiomyopathies, coronary artery disease, and atrial fibrillation. Few studies have evaluated genetic determinants of LV diastolic function.
Methods
We meta-analyzed genome-wide association studies (GWAS) for seven quantitative LV diastolic traits measured by echocardiography using data from the Copenhagen Hospital Biobank and previously published GWAS from the EchoGen consortium. Analyzed traits included transmitral flow velocities (E- and A-wave, E/A ratio), E-wave deceleration time, tissue Doppler parameters (average e’, E/e’), left atrial (LA) diameter. We investigated if lead variants were reported in published GWAS for cardiometabolic traits. We next evaluated genetic correlations (rg) between diastolic traits and published GWAS for cardiomyopathies, heart failure subtypes, and MRI-derived diastolic function traits from the UK Biobank.
Results
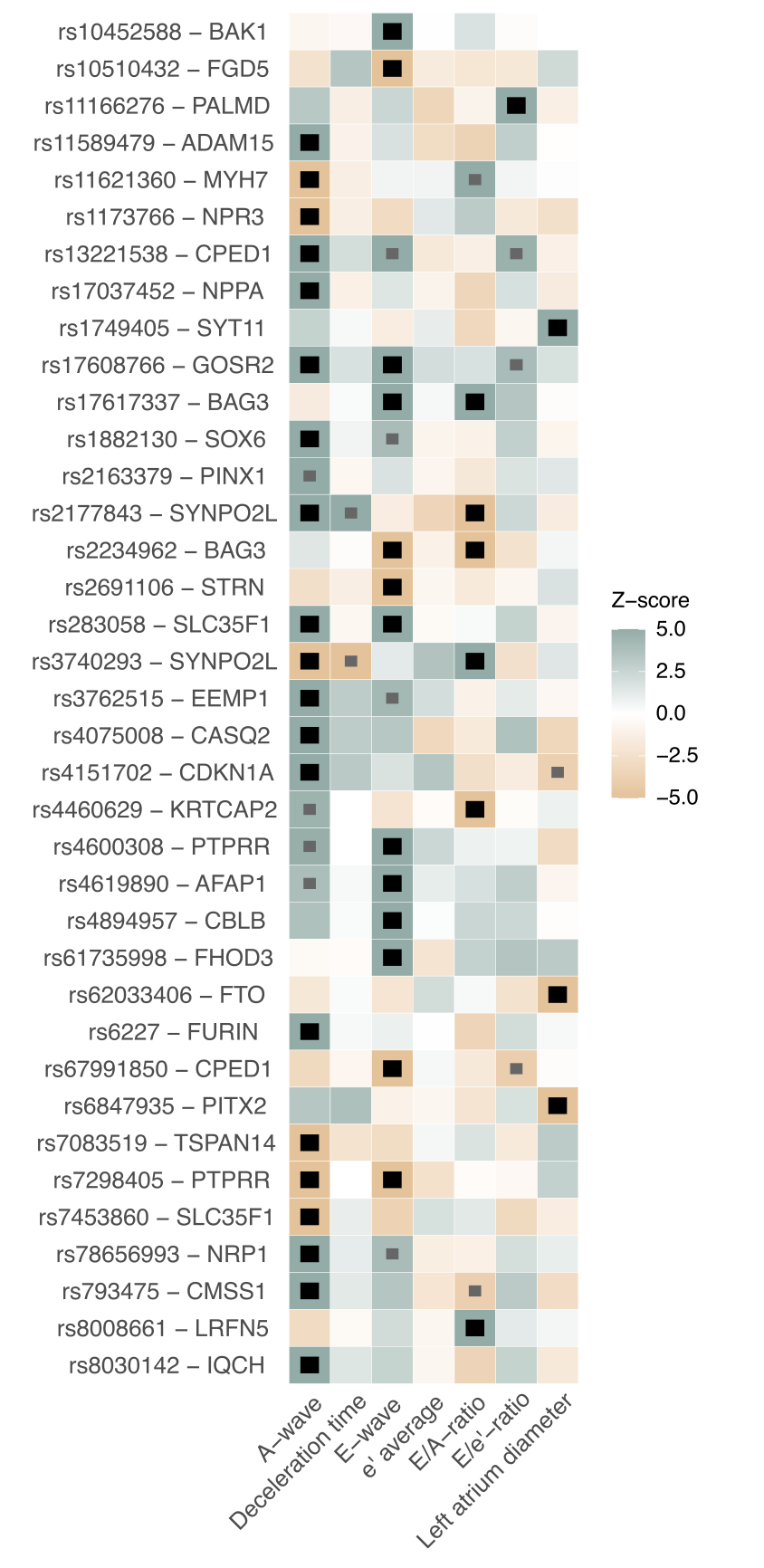
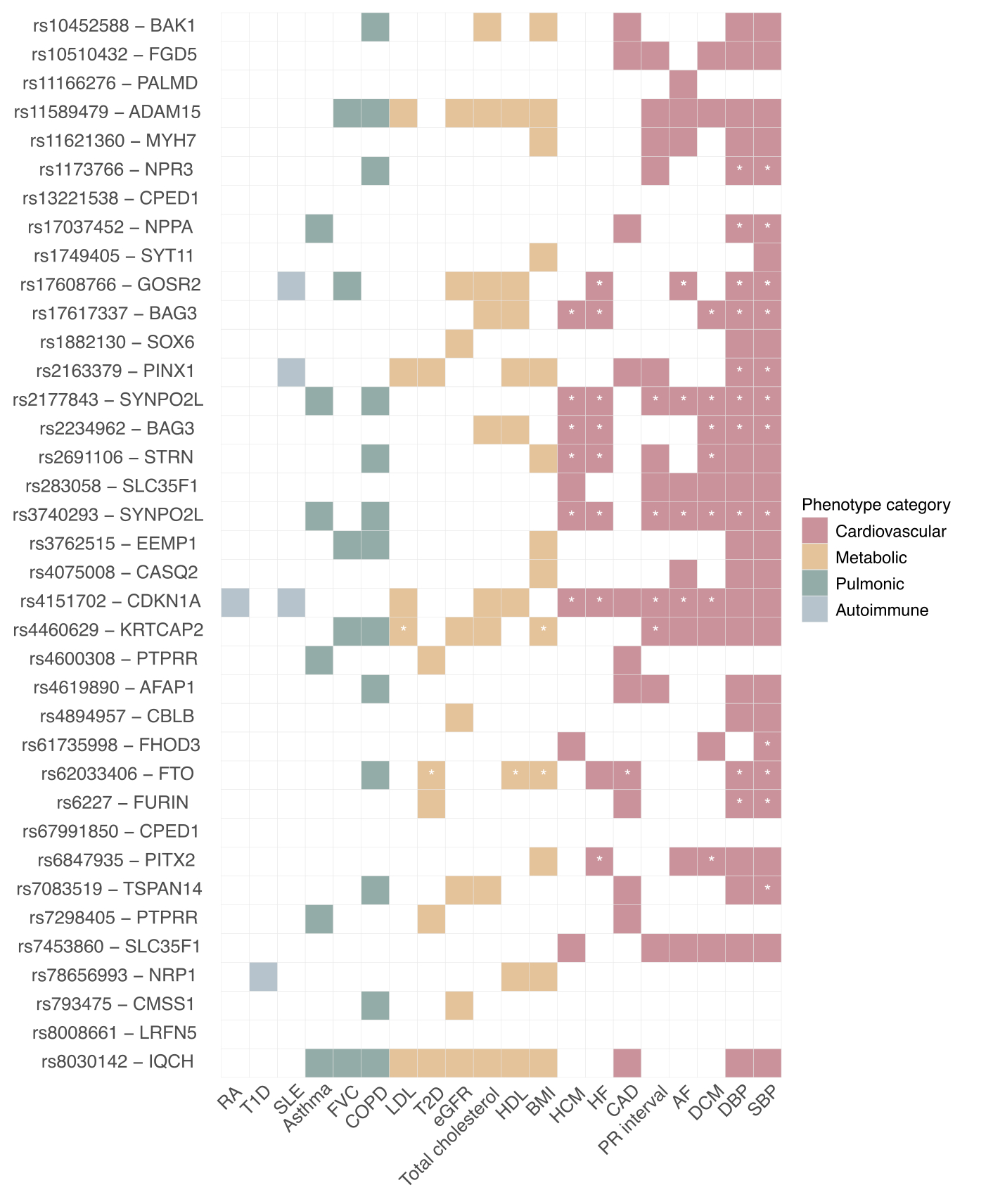
Using up to 72,093 individuals for genetic discovery, we identified 37 genome-wide significant independent loci associated with five of seven meta-analyzed traits (Fig.1). Lead variants overlapped with several published cardiometabolic risk loci, most prominently hypertensive traits. Several other were previously implicated in cardiomyopathies (MYH7, BAG3, SYNPO2L, PITX2, FHOD3, STRN, SYNPO2L, CDKN1A; Fig.2), and we also found loci near calcium-handling genes (PLN, CASQ2) and natriuretic peptide signalling genes (ANNP, NPR3). Several LV diastolic traits had strong genetic correlation to cMRI-derived traits (rg range from 0.60 [between E/A-ratio and LV strain] to 0.98 [between average e’ and LA passive emptying fraction]; all P < 1.5×10-5). LA diameter, E- and A-wave had moderate genetic correlation with cardiomyopathies, including HFpEF (rg range 0.31 – 0.54; all P < 0.01).
Conclusion
Common genetic variation plays a role in several key components of diastolic function, and are partly underpinned by variants near sarcomere, calcium-handling, and natriuretic signalling genes. Genetic correlation demonstrated that increased early and late diastolic filling as well as increased left atrial diameter positively correlated to HFpEF. Our findings indicate the variety of biological pathways contributing to cardiac diastolic function
Left ventricular (LV) diastolic function relies on active myocardial relaxation and passive cardiac chamber stiffness and is assessed by echocardiography. Abnormal LV diastolic function portends worse outcomes in heart failure (HF), cardiomyopathies, coronary artery disease, and atrial fibrillation. Few studies have evaluated genetic determinants of LV diastolic function.
Methods
We meta-analyzed genome-wide association studies (GWAS) for seven quantitative LV diastolic traits measured by echocardiography using data from the Copenhagen Hospital Biobank and previously published GWAS from the EchoGen consortium. Analyzed traits included transmitral flow velocities (E- and A-wave, E/A ratio), E-wave deceleration time, tissue Doppler parameters (average e’, E/e’), left atrial (LA) diameter. We investigated if lead variants were reported in published GWAS for cardiometabolic traits. We next evaluated genetic correlations (rg) between diastolic traits and published GWAS for cardiomyopathies, heart failure subtypes, and MRI-derived diastolic function traits from the UK Biobank.
Results
Using up to 72,093 individuals for genetic discovery, we identified 37 genome-wide significant independent loci associated with five of seven meta-analyzed traits (Fig.1). Lead variants overlapped with several published cardiometabolic risk loci, most prominently hypertensive traits. Several other were previously implicated in cardiomyopathies (MYH7, BAG3, SYNPO2L, PITX2, FHOD3, STRN, SYNPO2L, CDKN1A; Fig.2), and we also found loci near calcium-handling genes (PLN, CASQ2) and natriuretic peptide signalling genes (ANNP, NPR3). Several LV diastolic traits had strong genetic correlation to cMRI-derived traits (rg range from 0.60 [between E/A-ratio and LV strain] to 0.98 [between average e’ and LA passive emptying fraction]; all P < 1.5×10-5). LA diameter, E- and A-wave had moderate genetic correlation with cardiomyopathies, including HFpEF (rg range 0.31 – 0.54; all P < 0.01).
Conclusion
Common genetic variation plays a role in several key components of diastolic function, and are partly underpinned by variants near sarcomere, calcium-handling, and natriuretic signalling genes. Genetic correlation demonstrated that increased early and late diastolic filling as well as increased left atrial diameter positively correlated to HFpEF. Our findings indicate the variety of biological pathways contributing to cardiac diastolic function
More abstracts on this topic:
Artificial Intelligence-Enabled Electrocardiogram for the Detection of Elevated Filling Pressure in Hypertrophic Cardiomyopathy and Cardiac Amyloidosis
Van Lerberghe Robin, Grogan Martha, Friedman Paul, Herrmann Joerg, Janssens Stefan, Vandenberk Bert, Jacobs Johanna, Servaes Veerle, Robyns Tomas, Van Aelst Lucas, Mangold Kathryn, Attia Zachi, Oh Jae
A Two-Hit HFpEF-like Mouse Model with Accelerated Disease OnsetNehra Sarita, Selvam Sabariya, Anand Amit, Luettgen Joseph, Gulia Jyoti, Dokania Manoj, Gupta Ankit, Garcia Ricardo, Dudhgaonkar Shailesh, Mazumder Tagore Debarati, Ck Neethu, Wagh Somnath, Kale Prajakta