Final ID: MP989
Influenza Vs COVID-19 and Arrhythmic Events. A Propensity Matched Analysis
Abstract Body (Do not enter title and authors here): Background
The cardiovascular and mortality outcomes of COVID-19 versus influenza remain under study. This study aimed to compare these outcomes using a large real-world dataset and robust statistical matching.
Methods
This retrospective cohort study used the TriNetX global health research network. Patients aged ≥40 years with lab-confirmed COVID-19 or influenza (from Jan 1, 2020, to Dec 31, 2021) were included. Those with co-infection were excluded. Propensity score matching (1:1), based on demographics, diagnoses, medications, and lab values, was used to balance baseline characteristics. Outcomes assessed over 3 years post-index included: all-cause mortality, cardiac arrhythmias, ventricular tachycardia, ventricular fibrillation, atrial fibrillation, atrial flutter, and heart failure. Analyses included risk comparisons, survival analyses (Kaplan–Meier), and hazard ratios.
Results
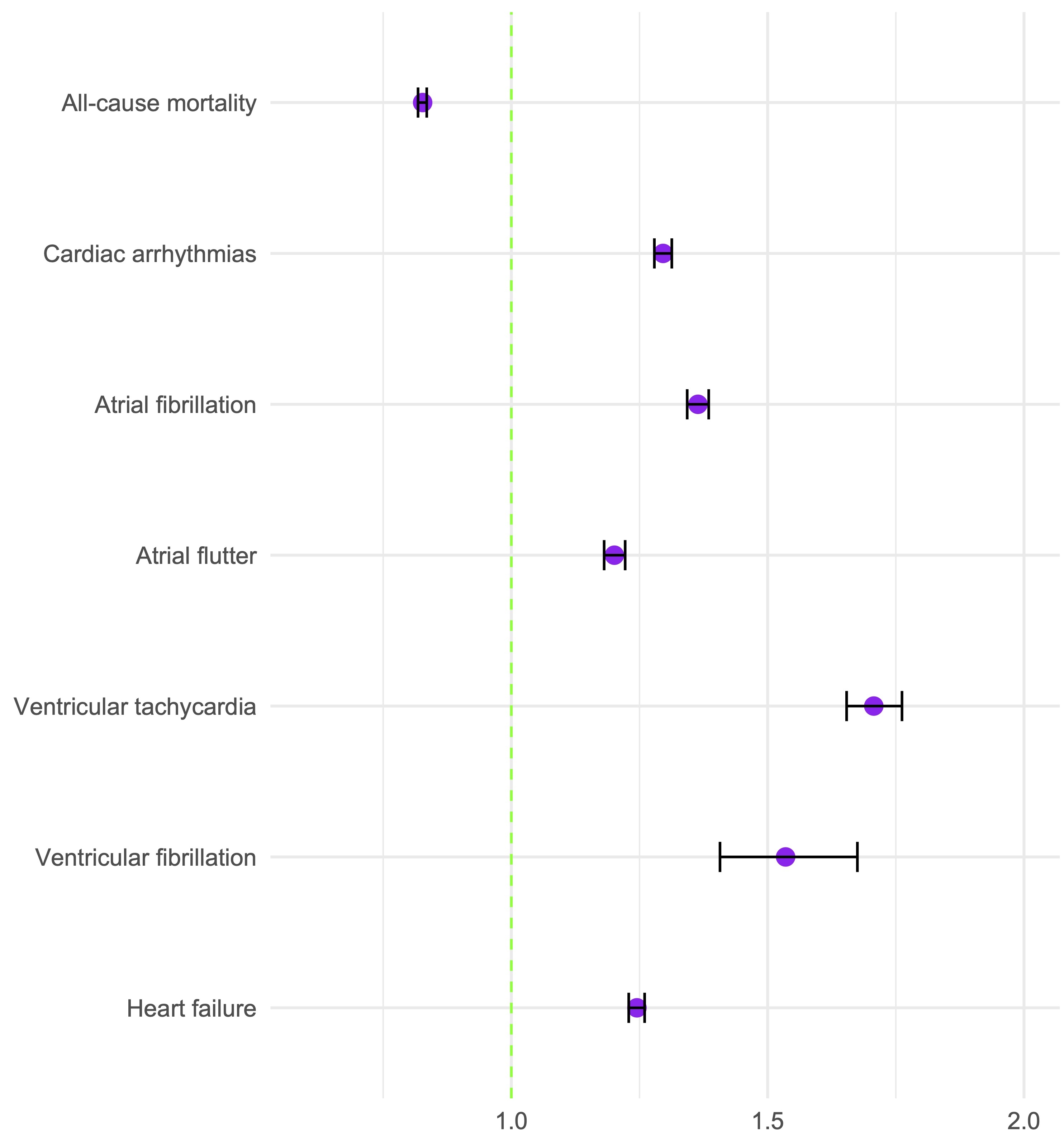
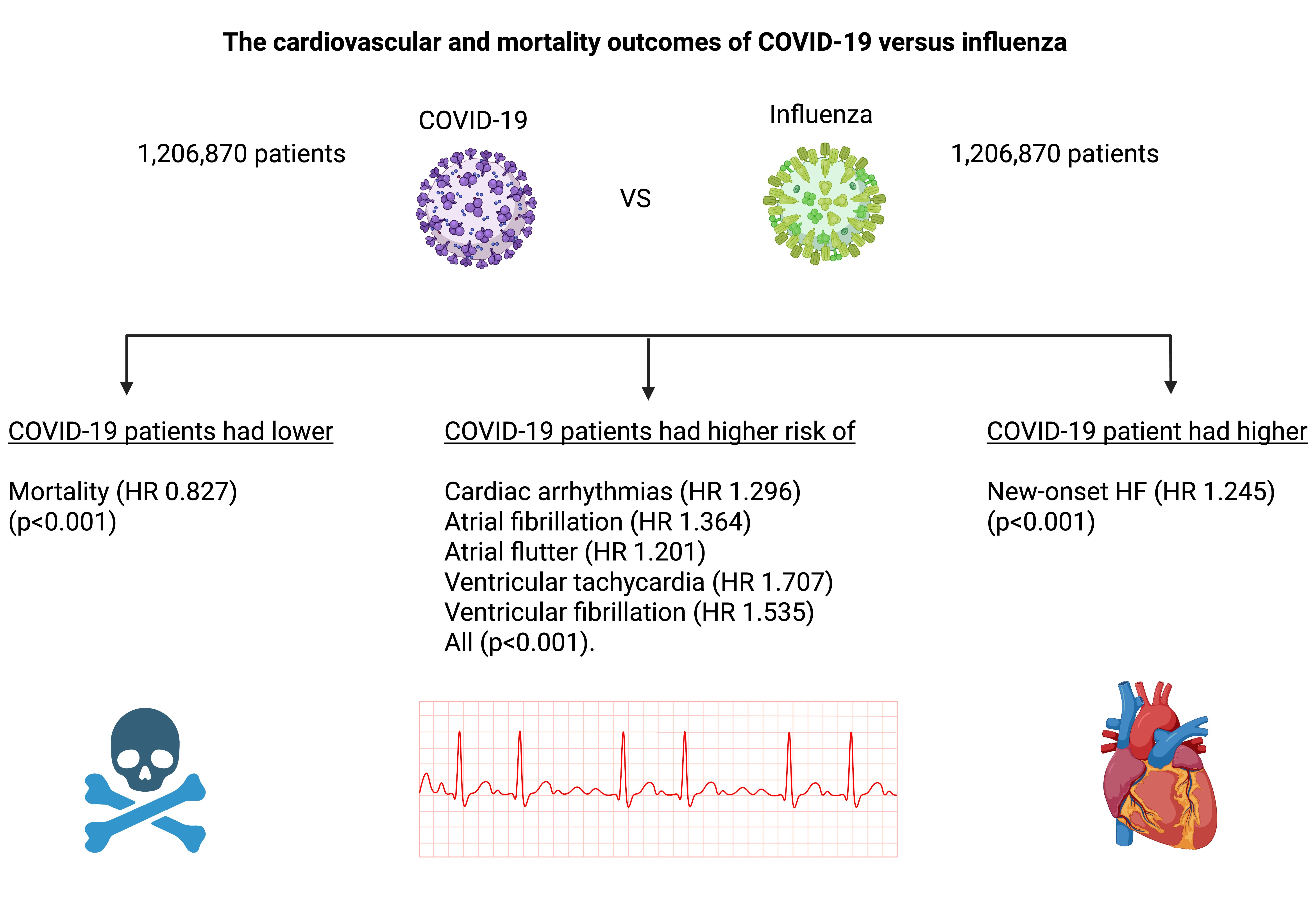
Among patients aged ≥40 years, COVID-19 (n=4,037,160) and influenza (n=1,270,965) cohorts were identified. Pre-matching, influenza patients had more comorbidities, including hypertension (24.8% vs. 16.2%), diabetes (10.8% vs. 6.5%), ischemic heart disease (6.1% vs. 4.2%), and heart failure (3.6% vs. 1.7%). COVID-19 patients had more chronic respiratory disease (17.3% vs. 10.6%). After 1:1 propensity score matching (n=1,206,870 per cohort), COVID-19 patients had lower mortality (HR 0.827, 95% CI: 0.818–0.835; p<0.001) but higher risk of cardiac arrhythmias (HR 1.296, 95% CI: 1.279–1.313; p<0.001), atrial fibrillation (HR 1.364, 95% CI: 1.343–1.385; p<0.001), atrial flutter (HR 1.201, 95% CI: 1.181–1.222; p<0.001), ventricular tachycardia (HR 1.707, 95% CI: 1.654–1.762; p<0.001), and ventricular fibrillation (HR 1.535, 95% CI: 1.407–1.675; p<0.001). New-onset heart failure was also higher in COVID-19 (HR 1.245, 95% CI: 1.229–1.260; p<0.001).
Conclusion
Despite a lower mortality rate, the COVID-19 group exhibited a consistently higher burden of arrhythmic events compared to the influenza group. These findings suggest distinct cardiovascular sequelae following COVID-19 infection, underlining the importance of post-acute surveillance in this population. Further studies are needed to understand the clinical implications.
The cardiovascular and mortality outcomes of COVID-19 versus influenza remain under study. This study aimed to compare these outcomes using a large real-world dataset and robust statistical matching.
Methods
This retrospective cohort study used the TriNetX global health research network. Patients aged ≥40 years with lab-confirmed COVID-19 or influenza (from Jan 1, 2020, to Dec 31, 2021) were included. Those with co-infection were excluded. Propensity score matching (1:1), based on demographics, diagnoses, medications, and lab values, was used to balance baseline characteristics. Outcomes assessed over 3 years post-index included: all-cause mortality, cardiac arrhythmias, ventricular tachycardia, ventricular fibrillation, atrial fibrillation, atrial flutter, and heart failure. Analyses included risk comparisons, survival analyses (Kaplan–Meier), and hazard ratios.
Results
Among patients aged ≥40 years, COVID-19 (n=4,037,160) and influenza (n=1,270,965) cohorts were identified. Pre-matching, influenza patients had more comorbidities, including hypertension (24.8% vs. 16.2%), diabetes (10.8% vs. 6.5%), ischemic heart disease (6.1% vs. 4.2%), and heart failure (3.6% vs. 1.7%). COVID-19 patients had more chronic respiratory disease (17.3% vs. 10.6%). After 1:1 propensity score matching (n=1,206,870 per cohort), COVID-19 patients had lower mortality (HR 0.827, 95% CI: 0.818–0.835; p<0.001) but higher risk of cardiac arrhythmias (HR 1.296, 95% CI: 1.279–1.313; p<0.001), atrial fibrillation (HR 1.364, 95% CI: 1.343–1.385; p<0.001), atrial flutter (HR 1.201, 95% CI: 1.181–1.222; p<0.001), ventricular tachycardia (HR 1.707, 95% CI: 1.654–1.762; p<0.001), and ventricular fibrillation (HR 1.535, 95% CI: 1.407–1.675; p<0.001). New-onset heart failure was also higher in COVID-19 (HR 1.245, 95% CI: 1.229–1.260; p<0.001).
Conclusion
Despite a lower mortality rate, the COVID-19 group exhibited a consistently higher burden of arrhythmic events compared to the influenza group. These findings suggest distinct cardiovascular sequelae following COVID-19 infection, underlining the importance of post-acute surveillance in this population. Further studies are needed to understand the clinical implications.
More abstracts on this topic:
A Simple One-Item Nursing Falls Assessment Predicts Outcomes For Patients With Stage D Heart Failure Undergoing Surgical Advanced Therapies
Salvador Vincent, Perez Jaime Abraham, Hudec Paige, Gorodeski Eiran, Oneill Thomas
A Beta Tubulin Mutation Suppresses Arrhythmias and Improves Connexin 43 Localization in Heart of Duchenne Muscular Dystrophy MiceZhou Delong, Liu Tong, Yehia Ghassan, Romanienko Peter, Rodney George, Wehrens Xander, Lampe Paul, Gourdie Robert, Xie Lai-hua, Fraidenraich Diego, Nouet Julie, Mesa Elam, Yegneshwaran Vasisht, Geukgeuzian Geovanni, Adibemma Ifeanyichukwu, Nandakumar Swetha, Ramirez Edwin, Li Hong