Final ID: Mo1014
Association of Framingham 10-year Cardiovascular Disease Risk Scores with Incident Probable Dementia and Cognitive Impairment in the SPRINT trial
Abstract Body (Do not enter title and authors here): Background: Cardiovascular disease (CVD) and cognitive impairment share several risk factors, which may explain the link between higher 10-year Framingham CVD risk score (FRS) and cognitive decline in the general population. However, this association remains less established in hypertensive patients.
Objective: This ad hoc analysis of the Systolic Blood Pressure Intervention Trial (SPRINT) examined the association between the 10-year FRS and incident probable dementia (PD), mild cognitive impairment (MCI), and a composite of both outcomes.
Methods: SPRINT enrolled adults aged ≥50 years with hypertension but without diabetes or prior stroke. Participants with baseline clinical dementia, prescribed dementia medications, or with missing FRS score components were excluded.The FRS was calculated using baseline age, sex, smoking status, total and HDL cholesterol, and systolic blood pressure, with diabetes status set to 'none' per trial eligibility. Incident PD and mild MCI were centrally adjudicated during follow-up. Using multivariable Cox regression hazards models, we assessed associations between baseline FRS—modeled both as a continuous (per 1% increase) and categorical (FRS >15%) variable—and cognitive outcomes.
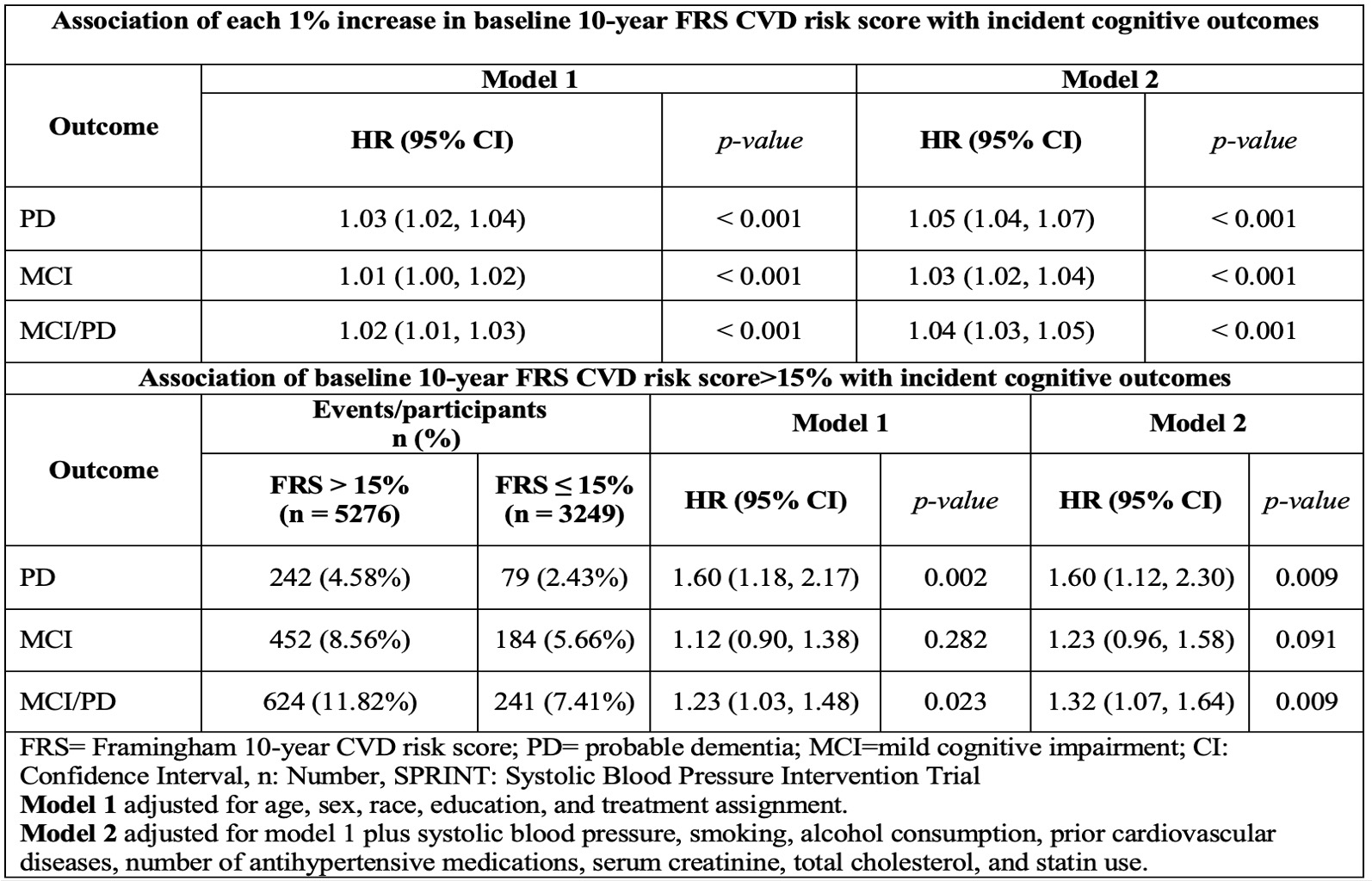
Results: Among 8,525 participants (mean age 67.9 years; 35.1% female) with complete FRS and cognitive outcome data, 5,276 (61.9%) had an FRS >15%. Over a median follow-up of 5 years, 321 cases (3.8%) of PD, 636 cases (7.5%) of MCI, and 865 cases (10.1%) of the composite outcome were identified. Incidence rates were significantly higher in participants with FRS >15% compared to those with lower FRS: PD (4.6% vs 2.4%), MCI (8.5% vs 5.6%), and the composite outcome (11.8% vs 7.4%). In multivariable Cox regression models adjusted for sociodemographic, treatment assignment, CVD risk factors, and other potential confounders, each percent increase in FRS was associated with a 5% increased risk of PD, a 3% of MCI, and a 4% increased risk of either outcome. In similar models, participants with FRS>15% had a 60% increased risk of PD, a 23% of MCI, and a 32% of either outcome compared to those with FRS<15% (Table).
Conclusion: Among hypertensive patients without diabetes or stroke, greater CVD risk burden as quantified by the FRS was significantly associated with elevated risks of both PD and MCI. Since most FRS components are modifiable, management of CVD risk factors could serve as a practical approach to maintain cognitive health in this high-risk population.
Objective: This ad hoc analysis of the Systolic Blood Pressure Intervention Trial (SPRINT) examined the association between the 10-year FRS and incident probable dementia (PD), mild cognitive impairment (MCI), and a composite of both outcomes.
Methods: SPRINT enrolled adults aged ≥50 years with hypertension but without diabetes or prior stroke. Participants with baseline clinical dementia, prescribed dementia medications, or with missing FRS score components were excluded.The FRS was calculated using baseline age, sex, smoking status, total and HDL cholesterol, and systolic blood pressure, with diabetes status set to 'none' per trial eligibility. Incident PD and mild MCI were centrally adjudicated during follow-up. Using multivariable Cox regression hazards models, we assessed associations between baseline FRS—modeled both as a continuous (per 1% increase) and categorical (FRS >15%) variable—and cognitive outcomes.
Results: Among 8,525 participants (mean age 67.9 years; 35.1% female) with complete FRS and cognitive outcome data, 5,276 (61.9%) had an FRS >15%. Over a median follow-up of 5 years, 321 cases (3.8%) of PD, 636 cases (7.5%) of MCI, and 865 cases (10.1%) of the composite outcome were identified. Incidence rates were significantly higher in participants with FRS >15% compared to those with lower FRS: PD (4.6% vs 2.4%), MCI (8.5% vs 5.6%), and the composite outcome (11.8% vs 7.4%). In multivariable Cox regression models adjusted for sociodemographic, treatment assignment, CVD risk factors, and other potential confounders, each percent increase in FRS was associated with a 5% increased risk of PD, a 3% of MCI, and a 4% increased risk of either outcome. In similar models, participants with FRS>15% had a 60% increased risk of PD, a 23% of MCI, and a 32% of either outcome compared to those with FRS<15% (Table).
Conclusion: Among hypertensive patients without diabetes or stroke, greater CVD risk burden as quantified by the FRS was significantly associated with elevated risks of both PD and MCI. Since most FRS components are modifiable, management of CVD risk factors could serve as a practical approach to maintain cognitive health in this high-risk population.
More abstracts on this topic:
Angiotensin-II Induced Hypertension Impairs the Brain Energy, Amino Acid and Lipid Metabolic Pathways
Ewees Mohamed, Amro Hani, Dodd Daniel, Abdelhady Ali, Gallego-perez Daniel, Zweier Jay, Hannawi Yousef
Adherence to Pediatric Screening Guidelines for Cardiovascular Risk Factors in a Diverse Cohort of Children in ChicagoGauen Abigail, Wang Yaojie, Perak Amanda, Davis Matthew, Rosenman Marc, Lloyd-jones Donald, Zmora Rachel, Allen Norrina, Petito Lucia