Final ID: MP2321
Protective Effect of Renin–Angiotensin–Aldosterone System Inhibitors Guided by Artificial Intelligence–Enabled Electrocardiograms on Incident Left Ventricular Dysfunction: A Multicenter Cohort Study
Abstract Body (Do not enter title and authors here): Background: Artificial intelligence–enabled electrocardiogram (AI-ECG) models can accurately detect left ventricular dysfunction (LVD), and their misclassification in patients with normal LV function may predict incident LVD. However, the prognostic value of AI-ECG and its role in guiding heart failure therapies, including angiotensin-converting enzyme inhibitors (ACEi) or angiotensin II receptor blockers (ARBs), remain insufficiently investigated.
Methods: This retrospective study included adults with baseline LVEF ≥ 50% on echocardiography who underwent ECG evaluation in a multicenter database of 10 hospitals from January 2016 to December 2024. A previously developed ECG-based algorithm stratified patients into high- and low-risk LVD groups. The primary outcome was incident LVEF ≤ 40% on follow-up echocardiograms. Propensity score matching and Cox proportional hazards models were used to estimate treatment effects, with follow-up through December 2024.
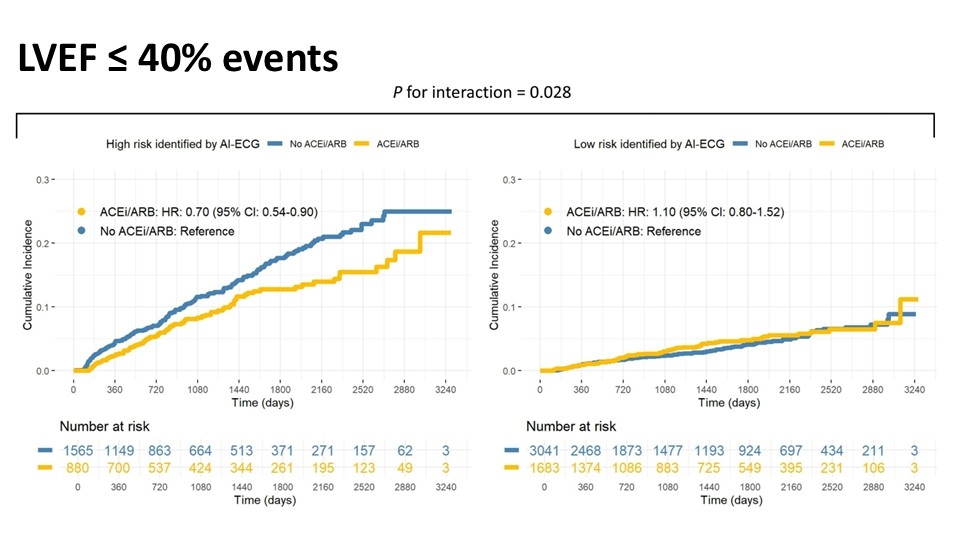
Results: After propensity score matching, 7,169 patients were analyzed (mean age 68 years; 55% male), including 1,683 low-risk and 880 high-risk patients who received ACEi or ARB therapy, and 3,041 low-risk and 1,565 high-risk patients who did not. Over a median follow-up of 1,320 days, the high-risk group had a significantly greater risk of incident LVEF ≤ 40% (hazard ratio [HR], 3.68; 95% confidence interval [CI]: 3.02–4.49). In the high-risk group, ACEi or ARB therapy was associated with a lower risk of LVEF decline compared to no treatment (HR, 0.70; 95% CI, 0.54–0.90); this effect was not observed in the low-risk group (HR, 1.10; 95% CI, 0.80–1.52; p for interaction = 0.028; Figure 1). Subgroup analyses confirmed the consistency of this finding across demographic groups, clinical settings, and comorbidities, and after adjusting for the competing risk of death.
Conclusion: AI-ECG effectively identified individuals at high risk for incident LVEF decline, and preemptive ACEi or ARB therapy was associated with a reduced risk of LVEF decline in this group. Further investigation is warranted to establish a causal relationship between ACEi/ARB therapy and AI-ECG–based risk stratification.
Methods: This retrospective study included adults with baseline LVEF ≥ 50% on echocardiography who underwent ECG evaluation in a multicenter database of 10 hospitals from January 2016 to December 2024. A previously developed ECG-based algorithm stratified patients into high- and low-risk LVD groups. The primary outcome was incident LVEF ≤ 40% on follow-up echocardiograms. Propensity score matching and Cox proportional hazards models were used to estimate treatment effects, with follow-up through December 2024.
Results: After propensity score matching, 7,169 patients were analyzed (mean age 68 years; 55% male), including 1,683 low-risk and 880 high-risk patients who received ACEi or ARB therapy, and 3,041 low-risk and 1,565 high-risk patients who did not. Over a median follow-up of 1,320 days, the high-risk group had a significantly greater risk of incident LVEF ≤ 40% (hazard ratio [HR], 3.68; 95% confidence interval [CI]: 3.02–4.49). In the high-risk group, ACEi or ARB therapy was associated with a lower risk of LVEF decline compared to no treatment (HR, 0.70; 95% CI, 0.54–0.90); this effect was not observed in the low-risk group (HR, 1.10; 95% CI, 0.80–1.52; p for interaction = 0.028; Figure 1). Subgroup analyses confirmed the consistency of this finding across demographic groups, clinical settings, and comorbidities, and after adjusting for the competing risk of death.
Conclusion: AI-ECG effectively identified individuals at high risk for incident LVEF decline, and preemptive ACEi or ARB therapy was associated with a reduced risk of LVEF decline in this group. Further investigation is warranted to establish a causal relationship between ACEi/ARB therapy and AI-ECG–based risk stratification.
More abstracts on this topic:
β1 Adrenergic Receptor Autoantibodies Promote Heart Failure Though Activation of Prostaglandin E2 Receptor EP1/Phosphodiesterase 4B Pathway
Cao Ning, Qiu Hui, Li Hongwei
A Case Presentation of Severe Left Ventricular Dysfunction from Focal Myocarditis due to Immune Checkpoint InhibitorPatel Romil, Hussain Kifah, Gordon Robert