Final ID: Su4027
Clinical Utility and Transethnic Calibration of Polygenic Risk Scores for Myocardial Infarction: A Global Meta-analysis Across Diverse Genetic Ancestries
Abstract Body (Do not enter title and authors here): Background: Polygenic risk scores (PRS) offer promising avenues for stratifying myocardial infarction (MI) risk and informing precision prevention. However, most PRS are derived from European-ancestry datasets, raising concerns about predictive validity and clinical equity across ancestrally diverse populations.
Goals/Aims: To evaluate the predictive performance, calibration, and clinical utility of MI-related PRS across global ancestries, and to identify strategies that enhance transethnic applicability.
Methods: We conducted a systematic review and meta-analysis in accordance with PRISMA guidelines. PubMed, Embase and Scopus were searched through March 2025 for studies reporting ancestry-stratified PRS performance for MI. Primary outcomes included area under the curve (AUC), odds ratio (OR) per standard deviation of PRS, observed-to-expected event ratios (O/E), and reclassification metrics (net reclassification improvement [NRI], integrated discrimination improvement [IDI]). Random-effects models were used for pooled estimates, with subgroup analyses by ancestry (European, African, South Asian, East Asian, Hispanic/Latino, admixed) and PRS construction method. Meta-regression, heterogeneity (I2), and risk-of-bias assessments were applied. Publication bias was evaluated via funnel plots and Egger’s test.
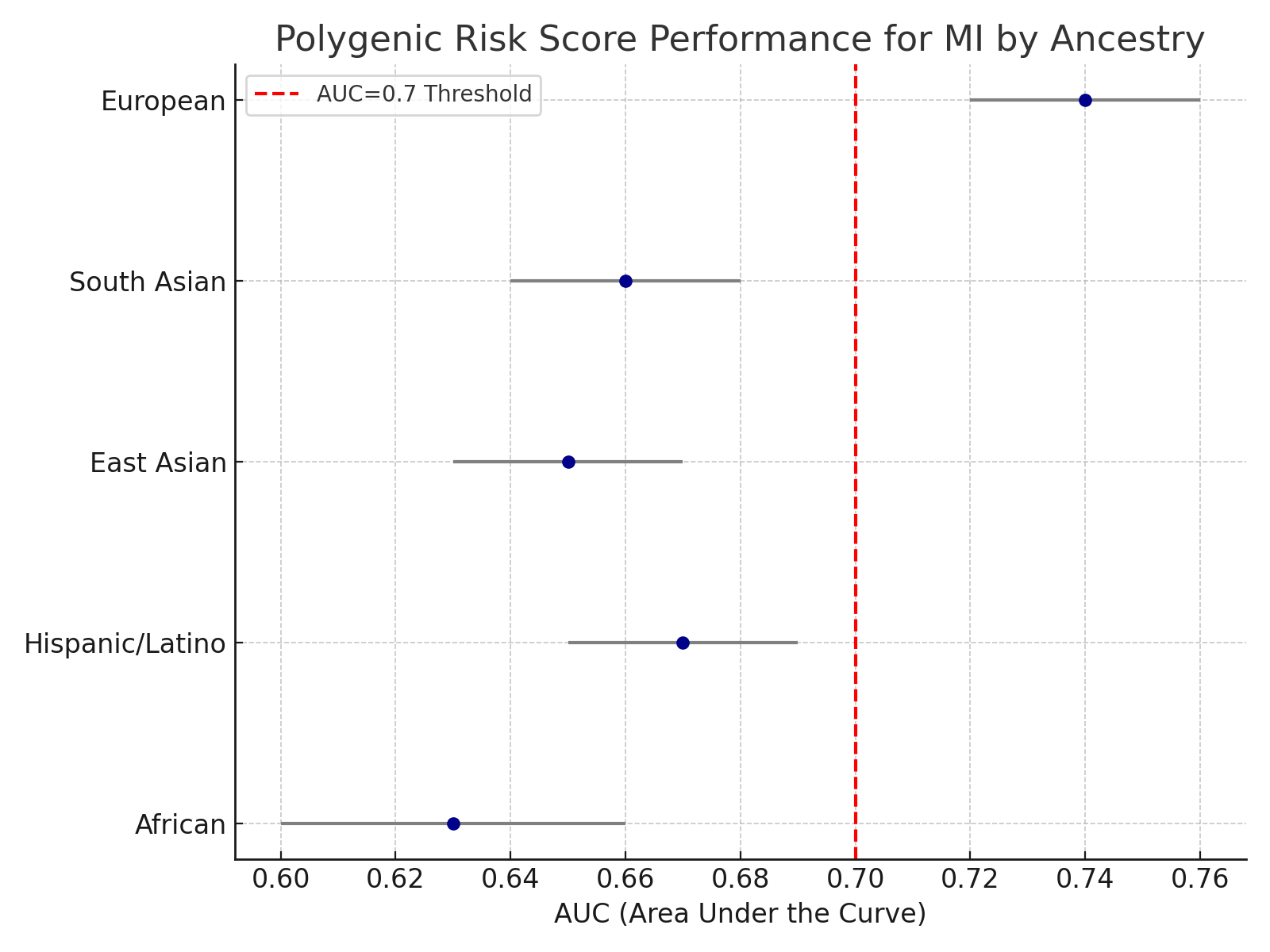
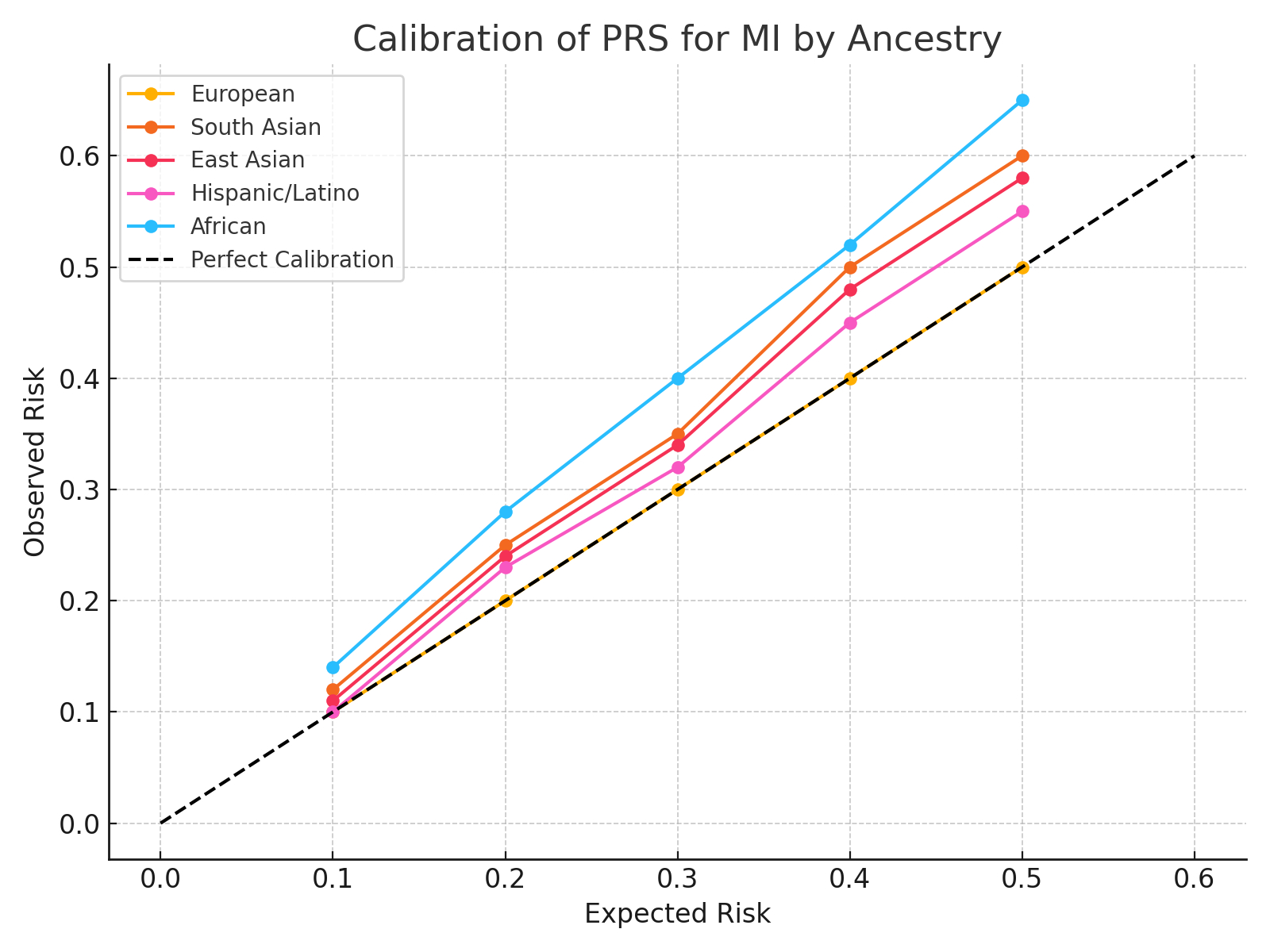
Results: Forty-six studies encompassing 1.32 million individuals across six ancestral groups were included. In European cohorts, pooled PRS AUC was 0.74 (95% CI: 0.72–0.76), compared to 0.63 (95% CI: 0.60–0.66) in African and 0.66 (95% CI: 0.64–0.68) in South Asian populations (p < 0.001 for heterogeneity). Calibration was poorer in non-European groups (O/E >1.4), indicating systemic overestimation of risk. While PRS improved net reclassification in European cohorts (NRI: +12.1%), clinical utility was limited in African ancestry (NRI: +2.3%). Meta-regression revealed that ancestry-specific allele frequency adjustment and inclusion of multi-ancestry training datasets significantly improved PRS performance (p < 0.01).
Conclusion: Current PRS for MI demonstrate reduced accuracy and suboptimal calibration in non-European populations, undermining clinical utility and exacerbating genomic health disparities. These findings highlight the urgent need for globally inclusive genomic data and ancestry-aware PRS optimization. Implementation of strategies is critical for equitable risk prediction tools and for aligning precision cardiology with global clinical practice.
Goals/Aims: To evaluate the predictive performance, calibration, and clinical utility of MI-related PRS across global ancestries, and to identify strategies that enhance transethnic applicability.
Methods: We conducted a systematic review and meta-analysis in accordance with PRISMA guidelines. PubMed, Embase and Scopus were searched through March 2025 for studies reporting ancestry-stratified PRS performance for MI. Primary outcomes included area under the curve (AUC), odds ratio (OR) per standard deviation of PRS, observed-to-expected event ratios (O/E), and reclassification metrics (net reclassification improvement [NRI], integrated discrimination improvement [IDI]). Random-effects models were used for pooled estimates, with subgroup analyses by ancestry (European, African, South Asian, East Asian, Hispanic/Latino, admixed) and PRS construction method. Meta-regression, heterogeneity (I2), and risk-of-bias assessments were applied. Publication bias was evaluated via funnel plots and Egger’s test.
Results: Forty-six studies encompassing 1.32 million individuals across six ancestral groups were included. In European cohorts, pooled PRS AUC was 0.74 (95% CI: 0.72–0.76), compared to 0.63 (95% CI: 0.60–0.66) in African and 0.66 (95% CI: 0.64–0.68) in South Asian populations (p < 0.001 for heterogeneity). Calibration was poorer in non-European groups (O/E >1.4), indicating systemic overestimation of risk. While PRS improved net reclassification in European cohorts (NRI: +12.1%), clinical utility was limited in African ancestry (NRI: +2.3%). Meta-regression revealed that ancestry-specific allele frequency adjustment and inclusion of multi-ancestry training datasets significantly improved PRS performance (p < 0.01).
Conclusion: Current PRS for MI demonstrate reduced accuracy and suboptimal calibration in non-European populations, undermining clinical utility and exacerbating genomic health disparities. These findings highlight the urgent need for globally inclusive genomic data and ancestry-aware PRS optimization. Implementation of strategies is critical for equitable risk prediction tools and for aligning precision cardiology with global clinical practice.
More abstracts on this topic:
Absence of standard modifiable risk factors (SMuRF-less) among 5002 Middle Eastern patients with atherosclerotic cardiovascular disease: (Interim analysis from the Jo-SMuRF Study)
Aldalal'ah Mo'men, Hammoudeh Ayman, Hamza Ibrahem, Alqudah Mohammad, Khasawneh Hasan, Alomari Sawsan, Alomari Ahmad, H. Assaf Sarah, Zaqqa Ayah, Khatatbeh Moawiah
A Novel Variant in GNB2 as a Cause of Sick Sinus SyndromeBulut Aybike, Karacan Mehmet, Saygili E. Alper, Pirli Dogukan, Aydin Eylul, Ozdemir Ozkan, Balci Nermin, Alanay Yasemin, Bilguvar Kaya, Akgun Dogan Ozlem