Final ID: MP600
The Impact of Neighborhood and Built Environment on Cardiovascular Health
Abstract Body (Do not enter title and authors here): Background: Cardiovascular disease (CVD) has remained the leading cause of death in the United States (US) for over a century. Despite progress in identifying risk factors and treatments, health disparities driven by social determinants of health (SDOH) remain underexplored. One key SDOH is the neighborhood and built environment, which influences cardiovascular (CV) health through behaviors and access to healthy food. This study examines how housing cost burden (HCB), a component of neighborhood and built environment, influences CV risk behaviors and outcomes in urban US zip codes.
Methods: Health data for urban zip codes of the US was extracted from the CDC PLACES database, which utilizes data from the Behavioral Risk Factor Surveillance System (BRFSS). HCB prevalence for each zip code was obtained from the American Community Survey (ACS) and divided into the following quartile ranges to ensure even distribution: low (0–19.5%), moderate (19.6–25.2%), high (25.3–32.6%), and severe (>32.6%). Descriptive statistics in R summarized the prevalence of health risk behaviors (binge drinking, smoking, short sleep duration, no leisure physical activity [PA]) and outcomes (diabetes [DM], hypertension [HTN], obesity, coronary heart disease [CHD], and stroke [CVA]) within each group. Kruskal-Wallis tests with Dunn’s post-hoc and univariate analysis assessed associations between HCB and CV outcomes.
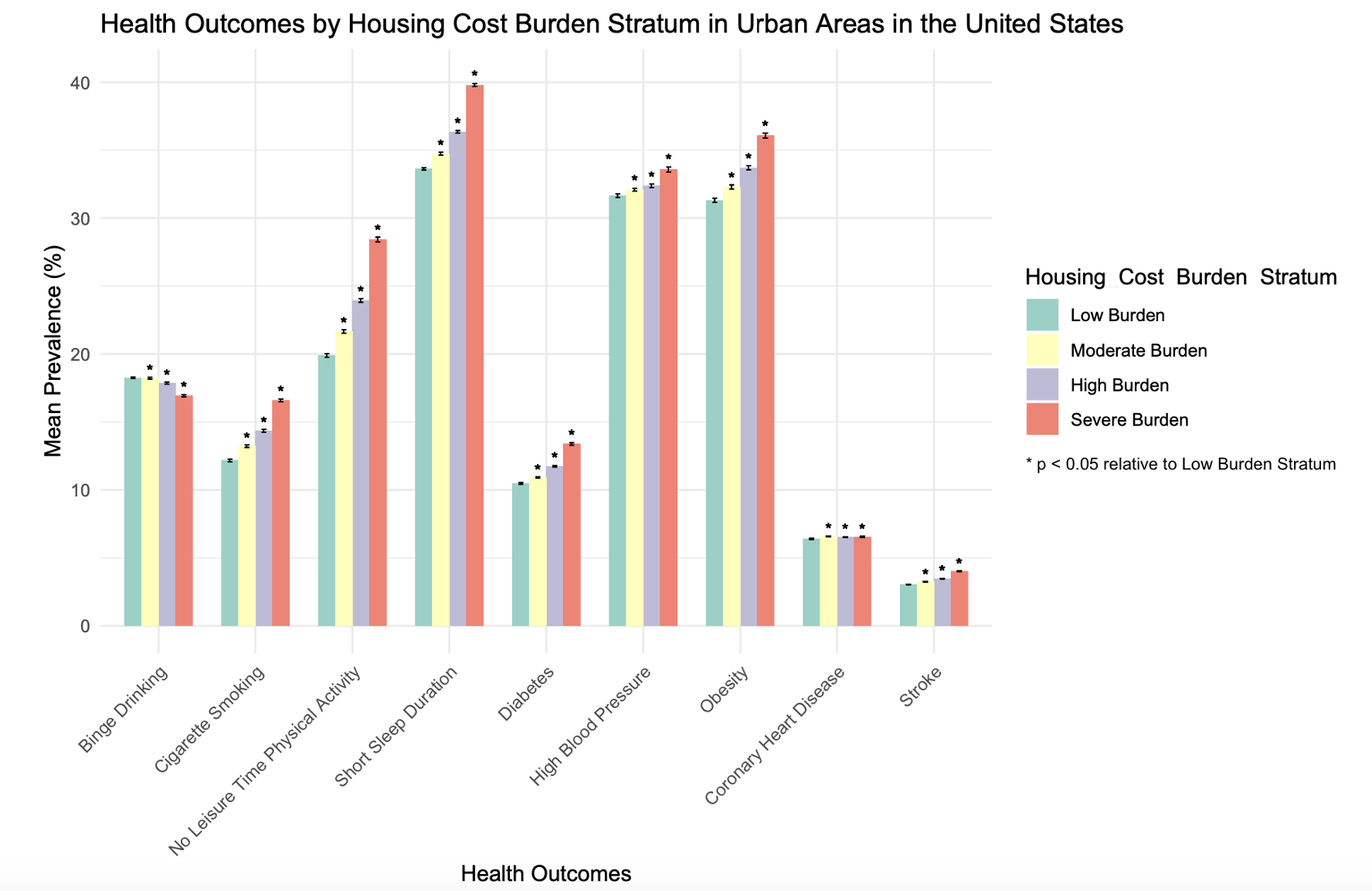
Results: Increased HCB was associated with higher rates cigarette smoking, shorter sleep duration, and lack of PA in urban zip codes of the US, shown in Figure 1 (p < 0.001, Kruskal-Wallis test). Higher HCB was also linked to increased prevalence of DM, HTN, obesity, CHD, and CVA, and lower rates of binge drinking (p < 0.001, Kruskal-Wallis test). A univariate regression analysis showed a similar positive association between HCB and cigarette smoking, physical inactivity, short sleep duration, DM, HTN, obesity, and CVA (p<0.001). However, no significant association was found between HCB and CHD (p = 0.213, univariate analysis). Interestingly, limiting the analysis to zip codes with populations over 5,000 resulted in a significant positive association between HCB and CHD (p = 0.041, univariate analysis).
Conclusion: HCB strongly correlates with CV risk behaviors and outcomes in urban US zip codes. These findings highlight the necessity of coupling social and medical care through approaches such as SDOH screening and public health interventions to advance equitable CV care.
Methods: Health data for urban zip codes of the US was extracted from the CDC PLACES database, which utilizes data from the Behavioral Risk Factor Surveillance System (BRFSS). HCB prevalence for each zip code was obtained from the American Community Survey (ACS) and divided into the following quartile ranges to ensure even distribution: low (0–19.5%), moderate (19.6–25.2%), high (25.3–32.6%), and severe (>32.6%). Descriptive statistics in R summarized the prevalence of health risk behaviors (binge drinking, smoking, short sleep duration, no leisure physical activity [PA]) and outcomes (diabetes [DM], hypertension [HTN], obesity, coronary heart disease [CHD], and stroke [CVA]) within each group. Kruskal-Wallis tests with Dunn’s post-hoc and univariate analysis assessed associations between HCB and CV outcomes.
Results: Increased HCB was associated with higher rates cigarette smoking, shorter sleep duration, and lack of PA in urban zip codes of the US, shown in Figure 1 (p < 0.001, Kruskal-Wallis test). Higher HCB was also linked to increased prevalence of DM, HTN, obesity, CHD, and CVA, and lower rates of binge drinking (p < 0.001, Kruskal-Wallis test). A univariate regression analysis showed a similar positive association between HCB and cigarette smoking, physical inactivity, short sleep duration, DM, HTN, obesity, and CVA (p<0.001). However, no significant association was found between HCB and CHD (p = 0.213, univariate analysis). Interestingly, limiting the analysis to zip codes with populations over 5,000 resulted in a significant positive association between HCB and CHD (p = 0.041, univariate analysis).
Conclusion: HCB strongly correlates with CV risk behaviors and outcomes in urban US zip codes. These findings highlight the necessity of coupling social and medical care through approaches such as SDOH screening and public health interventions to advance equitable CV care.
More abstracts on this topic:
Adverse Childhood Experiences (ACEs) and Cardiovascular Health: Future of Families and Child Wellbeing Study (FFCWS)
__PRESENT
__PRESENT
Pedamallu Havisha, Van Horn Linda, Stein James, Korcarz Claudia, Hansen Kristin, Mitchell Colter, Heard-garris Nia, Lloyd-jones Donald, Allen Norrina, Gauen Abigail, Ning Hongyan, Wilkins John, Goldman Noreen, Notterman Daniel, Hou Lifang, Zheng Yinan, Marma Amanda
A Focus for Improvement - Factors for Lab Adherence in a Pediatric Preventive Cardiology ProgramHolsinger Hunter, Porterfield Ronna, Taylor Makenna, Dresbach Bethany, Seipel Brittany, Igwe Chukwuemeka, Alvarado Chance, Tran Andrew